Projects
INGO Grant Management
2025-35 – Family-Type Children’s Home (FTСH) for children with developmental disabilities
1. FTCH “Happy Child – Happy Family”

Family-Type Home: Where Hope Thrives for Children Bearing the Heaviest Burdens
The Ukrainian Dzus family, mother Nataliya and father Yuriy, consists of 14 members (as of September 1, 2025). They have 12 children: 5 biological and 7 adopted, with the oldest being 29 years old and the youngest only 2.5 years old.
In the foreseeable future, the family may welcome 2 more children (twins) from a sibling group already under their guardianship, expected to be born in September 2025.
From a legal perspective, this is a large foster/adoptive family that does not yet have the official status of a Family-Type Children’s Home (DBST). Obtaining this legal status is one of the family’s top priorities and will require support from the charitable foundation.

The family adopted their first children in 2020. Just before Russia’s full-scale invasion of Ukraine, they bought a large, long-awaited home in the suburbs of Kyiv—a dream they had cherished for many years. They celebrated their housewarming on February 20, 2022, only three days before enemy bombs began to fall on the city.
Their home was located right next to the tragically renowned Bucha, a place forever associated with the inhuman cruelty and barbarism of Russian forces. In the first days of the occupation, mother Nataliya escaped on foot through the fields with nine children in her care. This story could fill a chapter of its own—a real-life thriller with a happy ending. Nataliya and the children reached Germany, where they were warmly welcomed and fully supported by the local community.
After the Kyiv region was liberated, the family returned to Ukraine, reunited with the father, and began settling into their new home. The horrors they had experienced seemed to transform the parents, strengthening their resolve and inspiring them to adopt a child who had lost his parents during the war.
That’s how baby Danylo joined the family. He was just six months old at the time, abandoned by his biological mother and living in a hospital. Later, the family found his biological siblings—an older brother and sister—who were living in different orphanages, and brought them home as well. Under Ukrainian law, children born to the same biological parents constitute a “sibling group” and must be placed together for adoption. For Nataliya and Yuriy, this was never an obstacle; they didn’t hesitate to take all the siblings.
In total, the family has now adopted 7 children, all with severe developmental disabilities
When the parents took the children from the orphanage, it was clear they were frail and in poor health. However, their official documents contained no mention of serious illnesses. Only after the children joined the family and underwent full medical examinations was it discovered that they all suffer from FAS/FASD (Fetal Alcohol Syndrome / Fetal Alcohol Spectrum Disorder) and organic brain damage, caused by the fact that their biological parents were alcohol- and drug-addicted.
These serious diagnoses did not deter the devoted parents. On the contrary, Nataliya and Yuriy concentrated all their efforts on the children’s treatment and rehabilitation. In addition to severe neurological conditions, the children were diagnosed with psychiatric, ophthalmological, gynecological, orphan (rare), and endocrine disorders — too many to list in full. All of these are severe, chronic, and difficult to treat.
Currently, the parents manage the children’s medical treatment, rehabilitation, and upbringing themselves, with help from their older children. Their home is a sanctuary — but it urgently needs stability, resources, and the legal recognition of a Family-Type Children’s Home (DBST) to ensure long-term protection for the children.
With donor support, the Dzus family can provide ongoing medical care, therapy, and a stable future for these children, giving them not just a home, but a chance at life.

2. Long-Term Comprehensive Support Program for Large Foster Families / Family-Type Children’s Homes for Children with Developmental Disabilities (2025–2035)
BACKGROUND
Child-care & mental-health reform in Ukraine (focus: children with developmental disabilities)
Current status / context (high level)
Ukraine has committed to a long-term deinstitutionalization agenda (shifting from residential institutions to family-based and community care), but progress has been uneven and the war has dramatically complicated reforms. Prior to the full-scale invasion there were already very high numbers of children in institutional care; the conflict worsened the situation and exposed gaps in alternative care capacity.
What changed because of the war
The 2022 invasion damaged health and social-care infrastructure (including psychiatric and psycho-neurological institutions) and triggered mass displacement of children — increasing the number of children without parental care and putting extra pressure on deinstitutionalization efforts. Mental-health services have lost staff, and many specialized facilities were attacked or damaged during hostilities.
Why children with developmental disabilities are especially at risk
- Children with complex developmental, mental-health or multi-system needs are often concentrated in institutional settings and rely on specialist teams that are scarce outside institutions. When institutions close or are disrupted, there are insufficient family-based alternatives (trained foster families, home-based specialists, community rehabilitation services) to absorb them safely.
- The war reduced local capacity to train, recruit and retain Special Needs Providers (therapists, nurses, early-intervention teams), creating a supply–demand gap for community services that are essential for successful deinstitutionalization.
Ukrainian Government Policy
Resolution of the Cabinet of Ministers of Ukraine; Regulations on October 31, 2018 №926
https://zakon.rada.gov.ua/laws/show/926-2018-%D0%BF?lang=en#Text
The Government has adopted a decision aimed at reducing the number of orphans and children deprived of parental care, including those with disabilities, as well as persons from among them, in institutional care facilities by placing them in small group homes and ensuring opportunities for such children to be raised in family-like settings.
In particular, a Model Regulation on Small Group Homes has been approved. These are social protection institutions intended for the long-term (residential) accommodation of orphans and children deprived of parental care, including children with disabilities, in family-like conditions, with the goal of socialization and preparation for independent living, as well as facilitating the return of children to their biological families or placement in family-based forms of care.
The establishment of small group homes will contribute to optimizing the network of facilities providing social services, accelerating the reform of institutional care and upbringing institutions, ensuring maximum access for children to services within the community, and strengthening the role and responsibility of local executive authorities and local self-government bodies for the situation of children and families with children.
One of the tasks of a small group home is to ensure that the child attends the nearest preschool or general secondary education institution according to the place of residence, including guaranteeing the right of a child with special educational needs to inclusive education and the receipt of educational services in accordance with an individual development program.
The creation of small group homes will also help strengthen the role and responsibility of local executive authorities and local self-government bodies for the situation of children and families with children.
Operational gaps donors should care about (programmatic implications)
- Insufficient foster/kinship capacity — thousands of additional trained foster families and specialized foster placements are needed to receive children leaving institutions.
- Shortage of community-based specialists — early-intervention teams, special education teachers, pediatric neurologists/psychiatrists, and home-based caregivers are scarce outside major cities. Funding must support training, supervision, and salary/top-up schemes to retain staff.
- Continuity of care for complex/rare conditions — children with multi-system needs require coordinated clinical pathways (genetics, immunology, rehabilitation) — this coordination is fragile and often absent in decentralised community models.
Financing of foster family homes (DBST) in Ukraine
The financing of foster family homes (DBST) in Ukraine remains insufficient and inconsistent, especially when it comes to supporting families raising children with developmental disabilities. Despite the declared course toward deinstitutionalization and the closure of orphanages, the state social protection system is still largely oriented toward institutional care, while community-based alternatives remain underfunded.
State subsidies for DBSTs are often limited to basic needs, without accounting for the cost of specialized medical care, rehabilitation, or inclusive education. Families raising children with disabilities frequently face bureaucratic barriers in obtaining targeted financial aid, while local budgets often lack the resources to cover these expenses in full.
As a result, DBSTs that take in children with special needs must rely on charitable assistance and donor support to ensure adequate living conditions, treatment, and education. Without increased targeted funding and systemic state support, there is a risk that the deinstitutionalization process will stall, leaving vulnerable children without access to family-based care and proper development opportunities.
LONG-TERM COMPREHENSIVE SUPPORT PROGRAM FOR LARGE FOSTER FAMILIES / FAMILY-TYPE CHILDREN’S HOME FOR CHILDREN WITH DEVELOPMENTAL DISABILITIES (2025–2035):
CASE STUDY of FTCH “Happy Child – Happy Family”

The program is designed for a 10-year duration, ensuring that the majority of participating children will reach adulthood by its completion.
The projected cost is indicative and based on data available prior to 2025. It does not account for inflation, SNP payroll taxes, or vehicle depreciation; rather, it reflects only the key and most urgent cost categories.These estimates also exclude ongoing expenses for food, clothing, utilities, and other day-to-day needs, which constitute a significant portion of the FTCH’s operating budget.
Abovementioned calculations are based on a household of 14 individuals, including 7 foster children, with the potential for the household composition to increase annually. Nonetheless, these estimates clearly indicate that the annual operating costs for a single Family-Type Children’s Home (FTCH) amount to no less than USD 150,000 per year.
Short closing line for the grant
Investing in family-based care and specialist teams, now will prevent lifelong exclusion for children with developmental disabilities — and will deliver far higher social and economic returns than rebuilding institutions.

Individual Case Management
2025 – UKR01
Urgent Need for Assistance
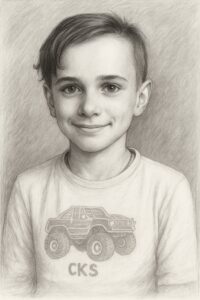
This is the story of a brave little boy named Alex, who is just 10 years old and lives in Kyiv, Ukraine. Unfortunately, Alex’s life is threatened not only by the war, but also by a severe medical condition he struggles with every single day.
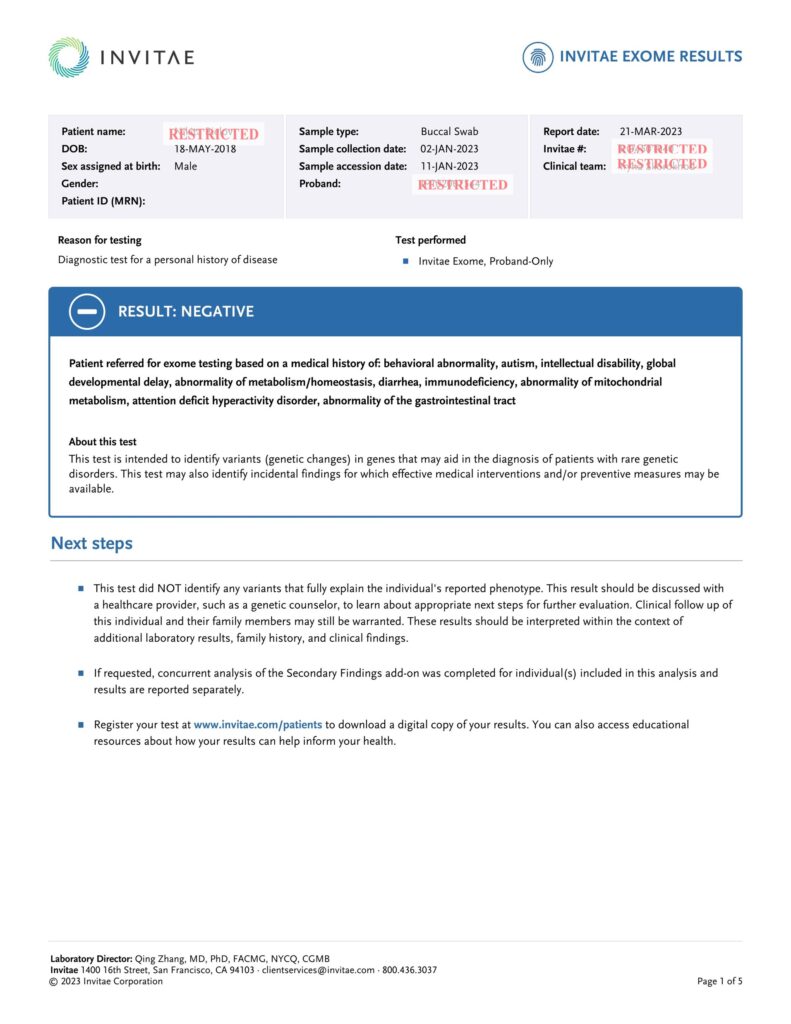
From the moment he was born, Alex has been fighting a difficult battle. He was diagnosed with a rare genetic disorder known as mTORopathy — a complex condition caused by a malfunction in a protein called mTOR, which plays a critical role in brain development.
This diagnosis affects many aspects of Alex’s life, including his cognitive and physical development, and requires constant medical supervision, therapies, and highly specialized treatment.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7726720/?utm_source=chatgpt.com#section3-1535759720959320
In simple terms:
mTORopathy is when mTOR doesn’t work properly—most often it’s too active—which causes the brain to develop abnormally. This can lead to: epilepsy, developmental delays, autism, and other neurological issues.
Why does this happen:
Normally, mTOR controls how brain cells grow and develop, especially in unborn babies and young children. But when a genetic mutation makes mTOR overactive, the brain grows too fast and in a disorganized way.
Examples of mTORopathies:
- Tuberous sclerosis — one of the best-known examples
- Focal cortical dysplasia (especially type II) — a brain malformation that causes epilepsy
- Some forms of epileptic encephalopathy in children
How is it diagnosed:
Diagnosing an mTORopathy involves several steps, combining clinical signs, brain imaging, genetic testing, and sometimes biopsy. Genetic Testing is key to confirming the diagnosis.
Types of tests:
- Targeted gene panels for mTOR pathway genes (e.g. TSC1, TSC2, MTOR, DEPDC5, PIK3CA, AKT3)
- Whole Exome Sequencing (WES) if the cause is unclear
- Somatic mutation testing (requires brain tissue, usually after epilepsy surgery)
How is it treated:
Since the main problem is too much mTOR activity, doctors use drugs that inhibit mTOR—such as Rapamycin or its derivatives (like Sirolimus). These medicines help: reduce mTOR activity, slow the growth of abnormal cells, lessen seizures, and improve overall function.
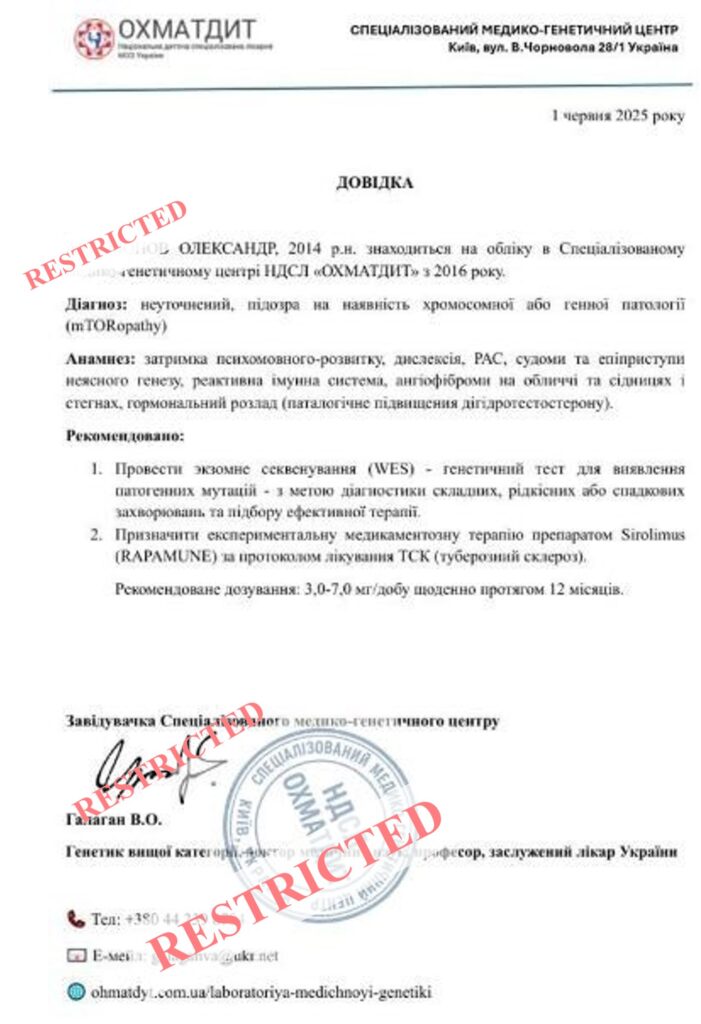
For many years, Alex has been under the care of the Specialized Medical-Genetic Center at “Ohmatdyt” National Children’s Hospital — the very same hospital that, one year ago, made headlines around the world.
In July 2024, a Russian ballistic missile struck and destroyed an entire building of Ukraine’s largest pediatric hospital. Miraculously, none of the young patients at “Ohmatdyt” were harmed. However, the hospital’s infrastructure suffered severe damage and has yet to be fully restored.
Sadly, neither “Ohmatdyt” nor the Ministry of Health of Ukraine currently has the resources to conduct advanced medical research or fund high-cost treatments.
Alex’s treatment protocol is extremely complex and costly, leaving a mother raising her son alone with no choice but to turn to a charitable foundation for help.
Treatment protocol:
- Genetic Test: Whole Exome Sequencing (WES) – $ 734 (one-off)
- Drug Therapy, Sirolimus (RAPAMUNE© Pfizer) – $ 24, 567 p.a.
https://www.drugs.com/price-guide/rapamune
The total cost of this Treatment protocol for one year is $25,300
Cost Estimation:
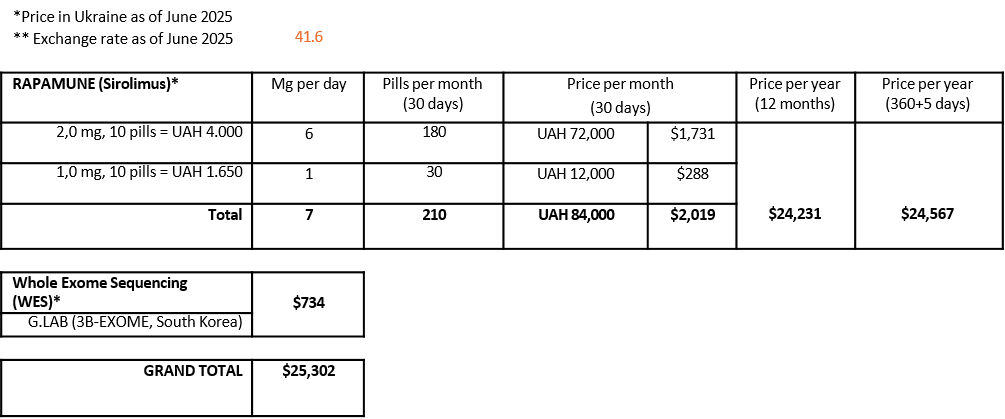
Alex began treatment with RAPAMUNE© in March 2025. After just three months of therapy, he has shown significant progress. That is why the treatment must not be interrupted under any circumstances — it is absolutely vital to his life and well-being.
Despite all the hardships of living under constant shelling in Kyiv, this year Alex completed the third grade at a general education school, keeping up with his peers. He dreams, he laughs, he fights — every single day. Here is why very contribution — no matter the size — brings Alex one step closer to stability, safety, and a better quality of life.

2025 – UKR09
This is a heartbreaking story of how war steals the last hope from gravely ill children and tears families apart
It is dedicated to little Vladik, who lives each day with autism and a rare autoimmune disorder, and to his devoted father, who carries the immense burden of raising and caring for his son alone.
Vladik is about to turn eight. He was born in Kyiv to loving parents and an older sister. From the very beginning, there were alarming signs — difficulties with feeding, irregular sleep, and noticeable developmental delays. He suffered from severe allergic reactions, including constant skin rashes, relentless itching, vomiting, and diarrhea when exposed to new foods. Frequent respiratory infections gradually progressed into chronic asthma. His cognitive and speech delays became more evident over time.
His parents responded immediately, seeking medical help and spending years visiting different doctors in hopes of finding answers. Vladik’s medical history is so extensive that it cannot fit on a single page.
On February 24, 2022, the full-scale war began. As bombs fell on Kyiv and across Ukraine, the family was forced to make an unbearable decision — to separate. Due to Vladik’s fragile condition, evacuation with other refugees was impossible. His mother took his sister and fled abroad. His father remained in Kyiv with Vladik, determined to care for him and eventually reunite the family.
In time, the mother settled in Germany and initially planned to bring Vladik to join them. Sadly, this never happened. The psychological toll of war seemed too heavy, and she ultimately chose to start a new life without her son. Two years later, the parents divorced, and Vladik’s father became his sole guardian.
The early years of the war meant that Vladik lost the opportunity for timely early intervention — a loss that would have lifelong consequences. By late 2023, he was diagnosed with autism spectrum disorder (F84.0), moderate intellectual disability (F71.0), and speech delay (F80.1). He was granted official disability status. However, his severe allergic and autoimmune condition remains largely undiagnosed and untreated to this day.
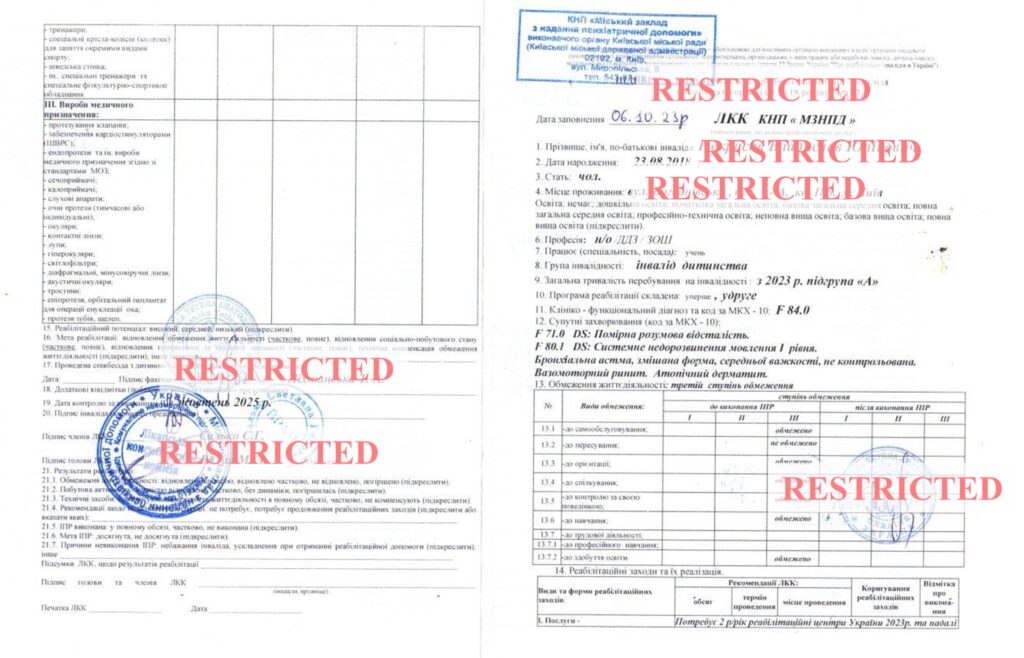
Today, Vladik’s father is the family’s sole provider. He works tirelessly, often traveling for work, just to cover basic living expenses. Vladik attends a state-run kindergarten which is open only in the mornings (9 AM–12 PM), and the quality of early intervention services provided there is far from sufficient. To give Vladik even a chance at future integration into society, the family relies on a team of private caregivers and developmental specialists.
The cost of Special Needs Providers’ support reaches $1,500 per month, or $18,000 per year.
In addition to the ongoing need for early intervention, Vladik urgently requires further medical evaluation. His father simply cannot afford the necessary diagnostic tests, which are essential for determining a treatment plan.
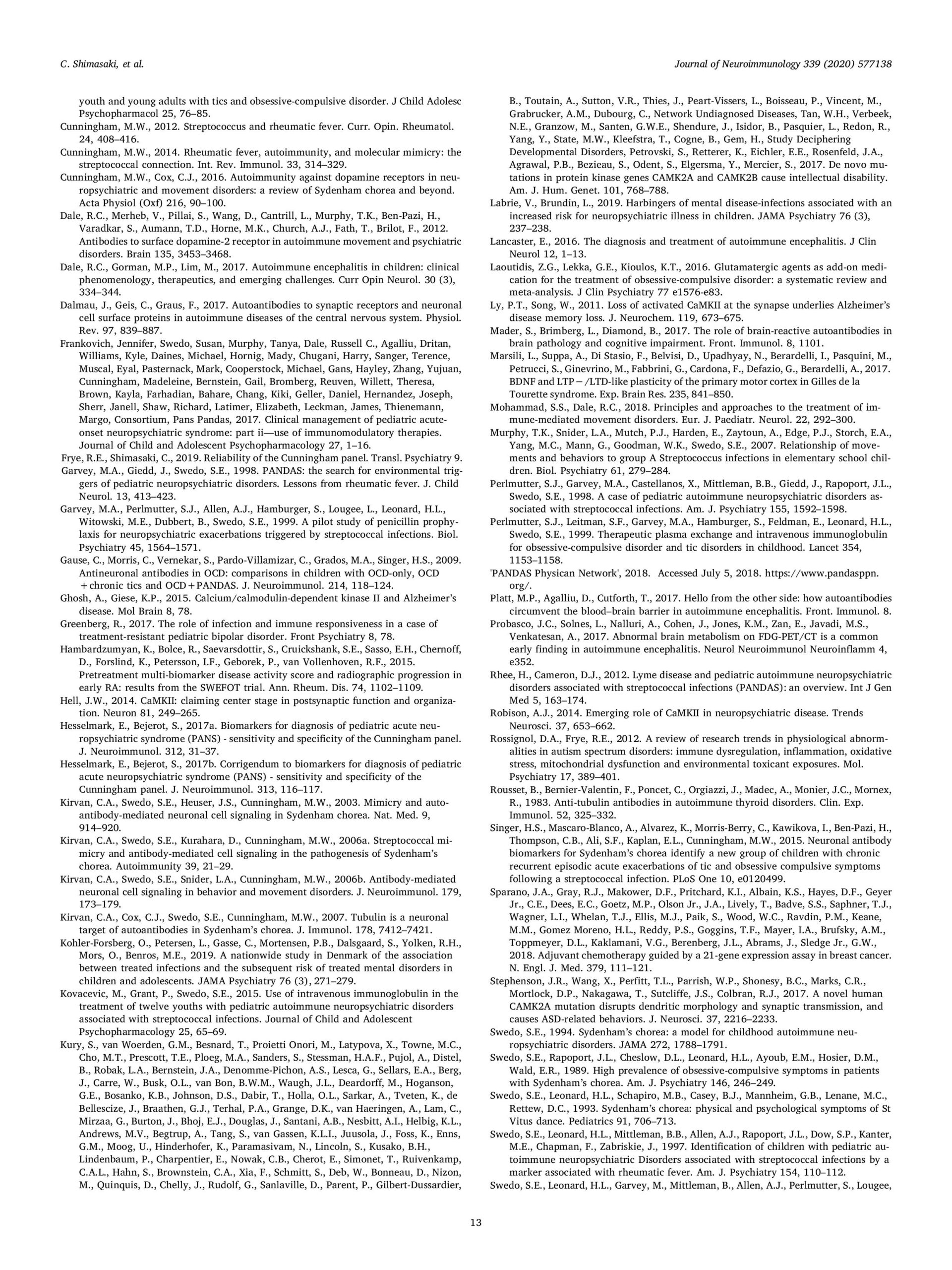
Phase 1 – Medical Diagnostics (Total: $2,100):
- Comprehensive Diagnostic Panel (CDP) – $1,100
- Whole Exome Sequencing (WES) – $1,000
Based on the findings from Phase 1, Phase 2 may involve further consultations and treatment in Ukraine or abroad, depending on the confirmed diagnosis.
Total Amount Needed for Phase 1: $21,100
This includes both the cost of ongoing early intervention and developmental support ($18,000 annually) and essential medical diagnostics ($2,100).
These funds will cover the team of private educators and caregivers who work with Vladik daily, as well as critical laboratory and genetic testing required to determine an accurate diagnosis and next steps in his treatment plan.

Vladik’s father is a deeply committed and loving parent.
He does everything in his power to ensure his son receives proper care and a chance at life.
He devotes all his free time to being with Vladik and is determined to give him a joyful and meaningful childhood, despite the enormous challenges they face.
In a society like Ukraine’s, where childrearing and medical caregiving are still overwhelmingly seen as the mother’s role, his dedication stands out — he deserves not only our respect, but our support.
No parent should carry this burden alone.
Let’s stand with Vladik — and with the father whose love and strength are helping him grow, thrive, and hold his head high.

2025 – UKR21
Unconditional Motherly Love
This is the story of a fragile Ukrainian mother carrying an unbearable burden with strength, grace, and unconditional love. Meet her son David — a 15-year-old boy from Kyiv, diagnosed with autism (F84.0) and delayed psycho-speech development (F71.1, F80.1).
In a cruel twist of fate, David was born as one of a pair of dizygotic twins. Although the boys look and behave very differently, only David carries a pathogenic genetic code that causes his condition. Yet, to their mother, they are equally cherished and the most precious children in the world.
Their father does not live with the family and plays no role in parenting. His financial support is far from sufficient to cover the high cost of care and treatment for a child with such a complex diagnosis.
Since birth, David’s mother has devoted herself entirely to his well-being. He has been seen by leading medical experts and worked intensively with private correctional educators and speech therapists. Despite some progress, David remains a complex and high-needs patient who requires round-the-clock supervision and specialized support.
David’s mother, a single parent, works full-time to provide for her two teenage sons. Once supported by her own mother — the boys’ grandmother — she now faces this journey alone, as the elderly woman has become increasingly frail and requires care herself. The immense weight of caregiving, financial responsibility, and emotional strain rests solely on this brave woman’s shoulders.
David’s condition has recently worsened. He is now in a state of persistent psychological hyperexcitability. Doctors are unsure whether this is due to disease progression or hormonal changes linked to puberty. David is now 5′7″ tall and weighs 132 lbs. During episodes of catatonic excitement, he becomes uncontrollably strong and can inadvertently harm himself or others.
Catatonic excitement is a severe psychomotor condition characterized by extreme, purposeless motor agitation, chaotic movements, verbal outbursts, and occasional aggression, all without clear external triggers. It is a psychiatric emergency.
Key features of catatonic excitement:
- Excessive, purposeless motor activity
- Repetitive or stereotyped movements
- Shouting, incoherent speech, or echolalia
- Increased muscle tone or resistance to movement (gegenhalten)
- Lack of responsiveness to the environment
- Possible self-injury or aggression toward others
These episodes have become overwhelming. David has destroyed their apartment, attacked his mother, his brother, elderly grandmother, and even his therapists. The family lives in constant fear, and finding appropriate Special Needs Providers (SNPs) has become an almost impossible task.
Sleep disturbances present another critical issue. David wakes up 10–12 times every night. His sleep phases are short and shallow, and he often wakes the entire household with noise, restlessness, and aggression. As a result, no one in the family is getting proper rest or functioning well during the day. Adding to the chaos are the frequent missile and drone attacks on Kyiv, which terrify David and further exacerbate his condition.
Currently, David attends a state-run medical facility for children with special needs. Unfortunately, it provides no treatment or therapeutic services. The mental health system in Ukraine is deeply underfunded, and reforms have been stalled by war. Authorities have suggested placing David in a remote residential institution. However, the conditions there are inhumane, and his loving mother refuses to abandon her son to such a place. Every day, she drives David to a specialized medical facility in Kyiv from 9 AM to 6 PM so that she can work.
Over the years, the family has consulted eight psychiatrists, including top specialists in Israel. David is currently on a regimen of neuroleptic medications, which have only marginally reduced the frequency and intensity of his episodes. The situation remains critical.
What Is Needed
Phase 1 – Emergency Support:
- Secure a second medical opinion from international specialists to explore innovative treatments for David’s sleep disturbances and aggressive hyperexcitation.
- Hire a Home-Based Mental Health Technician (MHT) — ideally a strong, trained male caregiver capable of assisting during both day and night crises.
Estimated cost: $750/month or $9,000 per year.
Phase 2 – Advanced Treatment Plan:
- Depending on the recommendations and the country of the specialist, this phase would cover:
- Multidisciplinary consultations;
- Additional diagnostic testing;
- Access to rare or costly medications if required.
At the very least, $9,000 annually is needed immediately to hire a home-based MHT and prevent the family from falling into complete physical and emotional collapse

This is a story of unwavering motherly love and unimaginable self-sacrifice. It’s about a small, fragile woman who has devoted her entire life to raising two sons — one of whom lives with a severe, complex disability — while also caring for her elderly mother. She bears this crushing responsibility alone: without rest, without a safety net, and with no one to lean on.
Mothers like her should never have to live this way — through sleepless nights, violent outbursts, relentless stress, and the constant fear of what tomorrow might bring for her child. She is a quiet hero, the embodiment of resilience, devotion, and unconditional love.
But love alone is not enough. She doesn’t just deserve our admiration — she needs and deserves real, tangible support.

Medical Programs
2025 – WES (Whole Exome Sequencing)
Whole Exome Sequencing (WES): A Lifeline for Ukraine’s Most Difficult-to-Diagnose Childhood Conditions
Whole Exome Sequencing (WES) is a powerful diagnostic tool that plays a vital role in identifying rare and complex genetic conditions — and it is increasingly in demand across Ukraine. However, the technical complexity of the procedure, the complete absence of in-country laboratories, and the high cost of analysis significantly limit access to this essential testing for Ukrainian families. To help bridge this gap, we are launching a special WES access program for 10 children with the most medically complex, undiagnosed cases. Thanks to the support of our donors, these children will receive WES testing free of charge, offering hope for an accurate diagnosis and a clearer medical pathway.
In selecting candidates for this program, we prioritize the most vulnerable categories: low-income families, single-parent households, families from the most war-affected regions of Ukraine etc. We focus on the most difficult and urgent medical cases, relying on a formal referral from the child’s treating physician. Additionally, every application is reviewed by the Foundation’s Commission, which includes independent medical experts — ensuring objectivity, fairness, and a trusted second opinion in every decision.
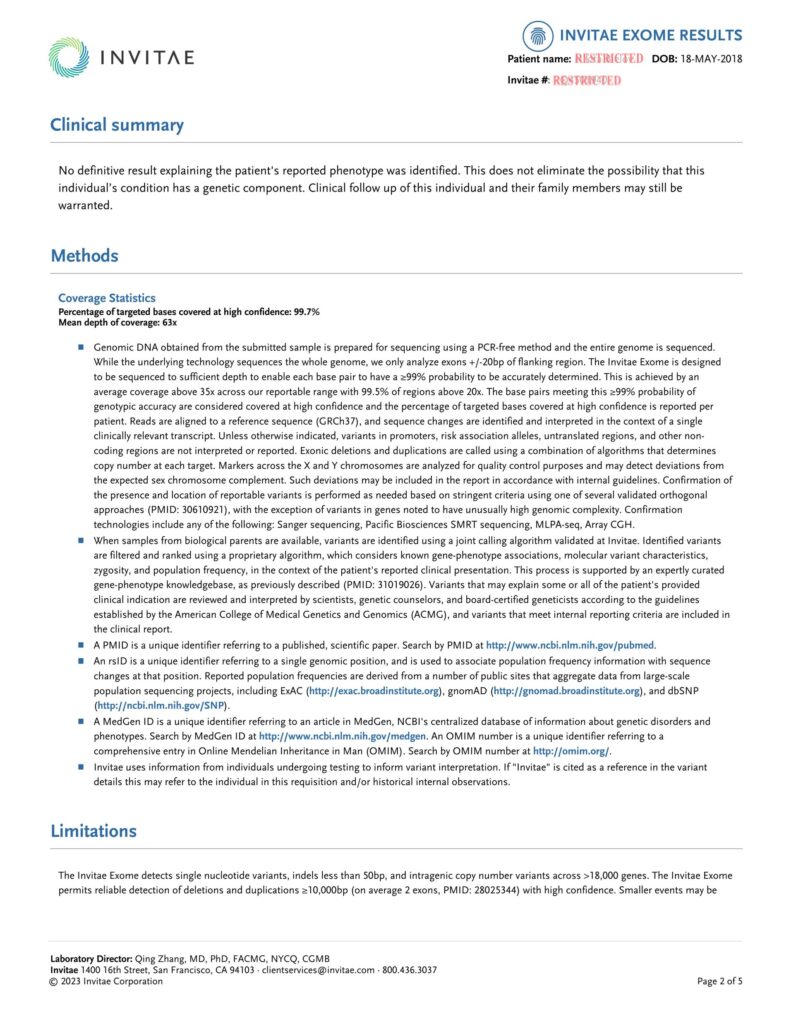
What is Whole Exome Sequencing (WES)?
Whole Exome Sequencing (WES) is a type of genetic test that analyzes the exome — the portion of the genome that contains all protein-coding genes. Although the exome makes up only about 1–2% of the entire human genome, it contains approximately 85% of known disease-related genetic mutations.
What is WES used for?
- Diagnose rare or unexplained genetic diseases, especially in children with complex medical conditions
- Identify mutations in single genes (monogenic disorders)
- Guide treatment decisions in some cases (e.g., personalized medicine or eligibility for clinical trials)
- Provide information for genetic counseling and family planning
Who may benefit from WES?
- Children with undiagnosed developmental delays, neurological disorders, or multiple congenital anomalies
- Patients with a suspected genetic condition that has not been identified through standard tests
- Families with a history of rare diseases or unexplained medical symptoms
Why WES is important for children with orphan (rare) diseases?
1. Fast and Accurate Diagnosis. Many rare diseases are genetic and caused by a single mutation in one gene. WES looks at all the protein-coding genes (the exome), where over 85% of disease-causing mutations are found. It can identify the cause of a child’s symptoms when other tests fail.
2. Reduces the Diagnostic Odyssey. Children with rare diseases often go through years of tests, misdiagnoses, and uncertainty. WES can shorten this journey dramatically by giving a diagnosis in one step.
3. Informs Treatment Options. Some rare diseases have targeted treatments or clinical trials — but only if the genetic cause is known. WES results can help doctors choose the right therapy or avoid harmful ones.
4. Opens the Door to Support. A confirmed diagnosis can help families access specialist care, support networks, educational resources, and financial aid. It also gives families peace of mind by finally understanding what their child is facing.
How is WES performed?
Whole Exome Sequencing (WES) testing in Ukraine is partially available, but still limited due to infrastructure, cost, and ongoing effects of the war. WES is not widely available in public hospitals. A few private medical centers in Kyiv, Lviv, and Dnipro offer access to genetic testing services in partnership with international labs. Ukrainian labs do not yet perform full WES in-country; samples are usually sent abroad (e.g., Germany, Austria, USA, or Israel). WES is not covered by the state, unless part of a research study or international humanitarian initiative.
Our team ensures transparency, medical accuracy, and support at every step. We work only with internationally certified laboratories and adhere to all bioethics and data protection standards.
COORDINATED ACROSS BORDERS – CENTERED ON THE CHILD
This cross-border WES process enables Ukrainian families to access cutting-edge genomic diagnostics while remaining in-country for all logistics and care coordination.
1. Initial Consultation & Medical Indications. The process begins with a consultation with a physician or genetic specialist to determine whether WES is medically indicated.
2. Biomaterial Collection in Ukraine. Certified Ukrainian medical centers collect the required biological samples — typically blood or saliva — from the patient and, when possible, both biological parents (for trio analysis). All procedures are performed under sterile, clinical conditions. Consent forms and medical records are prepared in both Ukrainian and English.
3. International Shipment to Accredited Genetic Labs. Samples are securely packaged and shipped via certified medical couriers (e.g., DHL Medical Express, FedEx Clinical Pak) to partner laboratories abroad — commonly in the United States, Germany, or Israel. Partner labs include CLIA/CAP-accredited institutions with expertise in advanced genome diagnostics.
4. Sequencing & Bioinformatic Analysis. At the laboratory, DNA is extracted and sequenced to identify variations across all coding regions of the exome.
5. Medical Report & Clinical Recommendations. Within 4–8 weeks, the family receives a comprehensive medical report, which includes:
- Pathogenic or likely pathogenic variants
- Variant of uncertain significance (if relevant)
- Clinical summary and explanation
- Treatment suggestions (if applicable)
- Recommendations for further testing or referrals
6. Post-Test Genetic Counseling. A follow-up consultation with a clinical geneticist is highly recommended to interpret the results, address family concerns, and outline next steps. Counseling may be done in person (Ukraine) or online (with international experts).
Cost of the medical service
The cost of Whole Exome Sequencing typically ranges from $700 to $5,000, and may be higher depending on the country, laboratory, and type of analysis performed.
The total cost of this Programme for 10 children with Invitae Corporation is $18,000
https://www.invitae.com/us/providers/test-catalog/test-80001
What Contributes to the High Cost of WES?
1. Advanced Technology. WES uses next-generation sequencing (NGS) machines, which are costly to buy, maintain, and operate. The lab processes require high-precision tools and skilled technicians.
2. Complex Data Analysis. After sequencing, a huge amount of genetic data (millions of base pairs) must be analyzed and interpreted. This step requires bioinformaticians and specialized software to detect and classify genetic variants.
3. Expert Review. Trained clinical geneticists and genetic counselors must review the results, determine if variants are harmful, and create a report. Many results are uncertain or rare, so the interpretation is time-consuming and requires expertise.
4. Quality Control & Validation. High standards are required to ensure accuracy, which adds time and cost. Some results may be double-checked using other methods (like Sanger sequencing) to confirm findings.
5. Customization. Every patient’s case is different. WES is not a one-size-fits-all test — the analysis is often tailored to the patient’s symptoms, family history, and clinical findings.
Despite all the challenges, Whole Exome Sequencing (WES) significantly simplifies the treatment process for Ukrainian children, provides clear answers to complex questions, and offers a ray of hope for full recovery.

2025 – Autoimmune Brain Panel™
Helping Children with Rare Autoimmune Brain Conditions
Including PANS/PANDAS, and other immune-mediated neuropsychiatric disorders
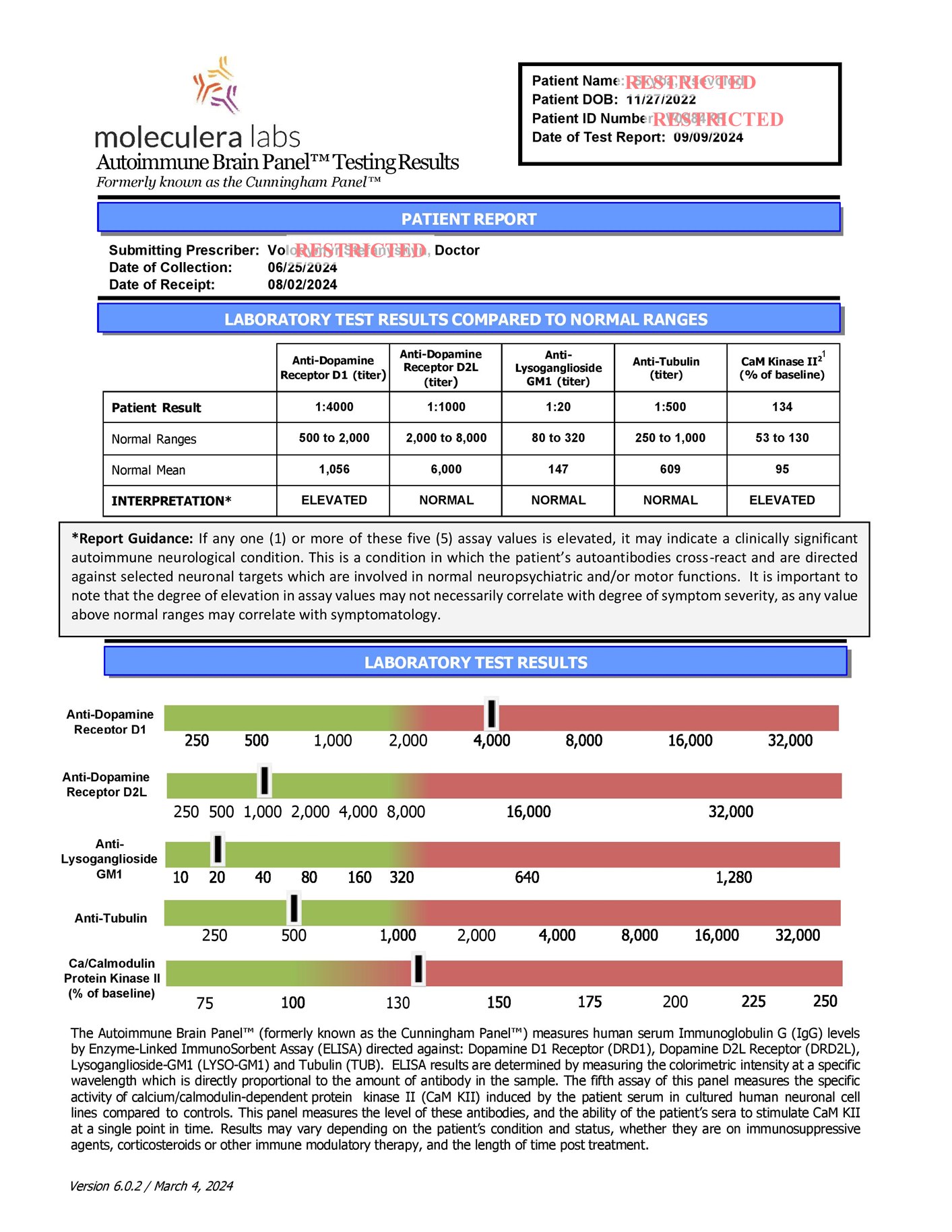
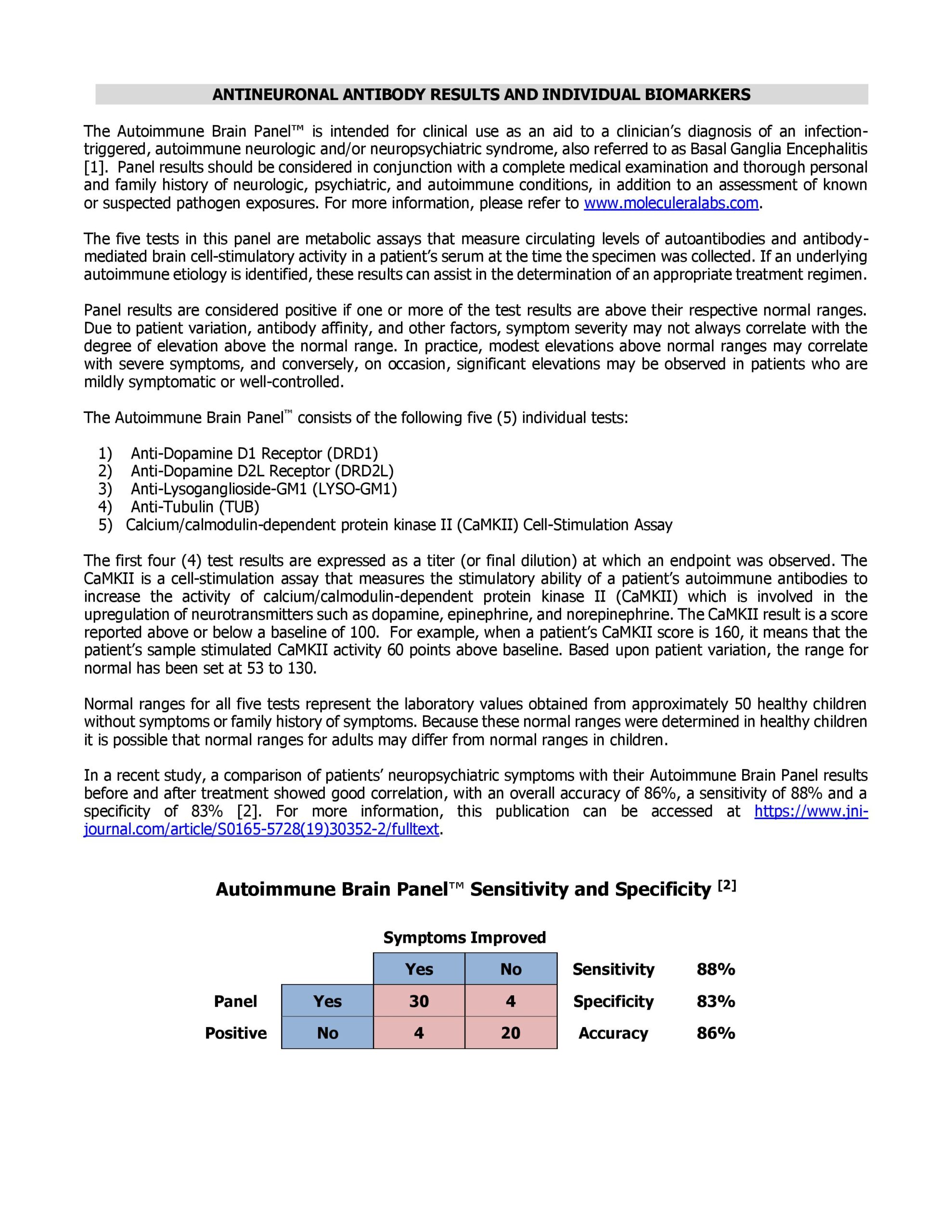
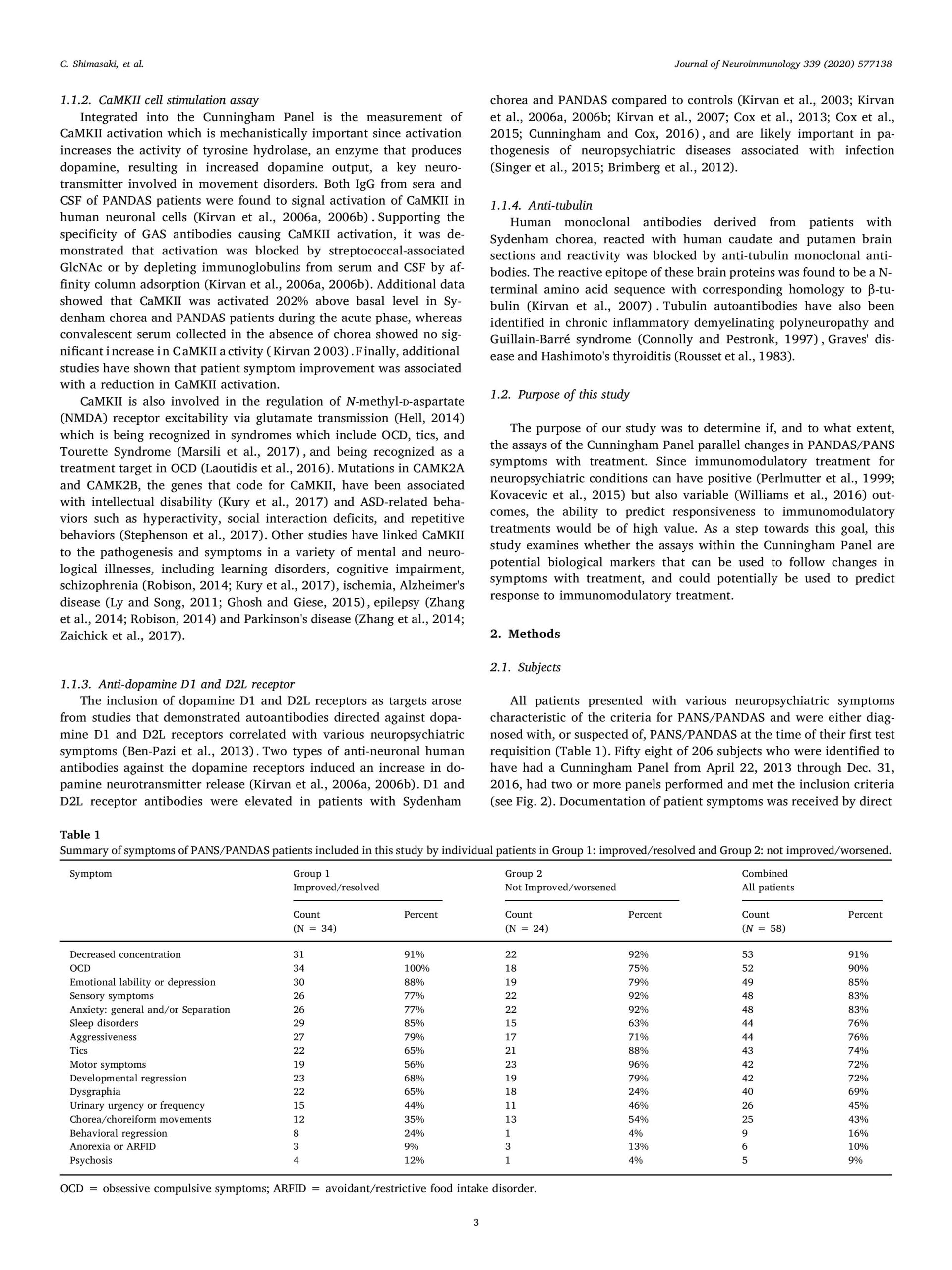
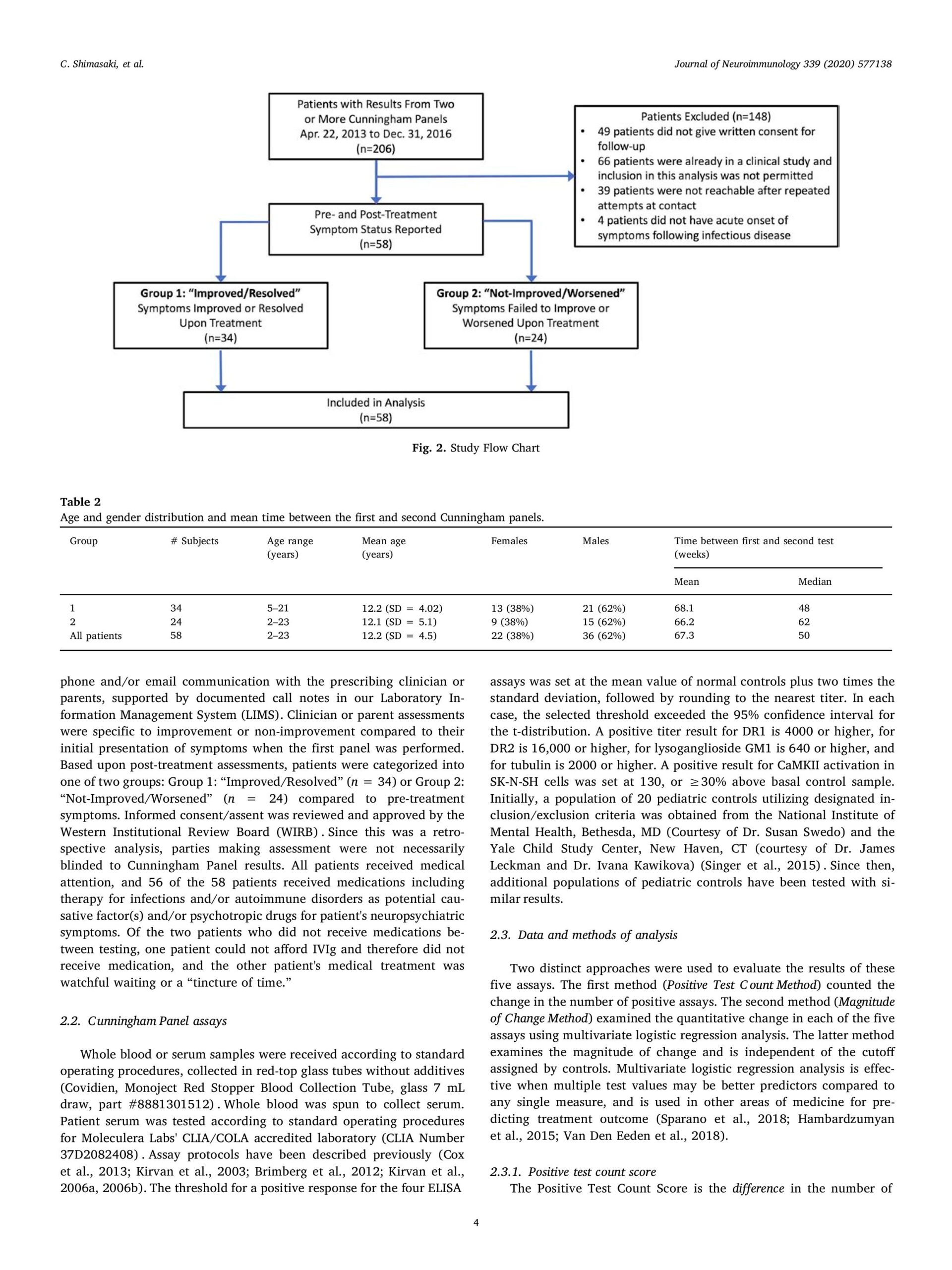
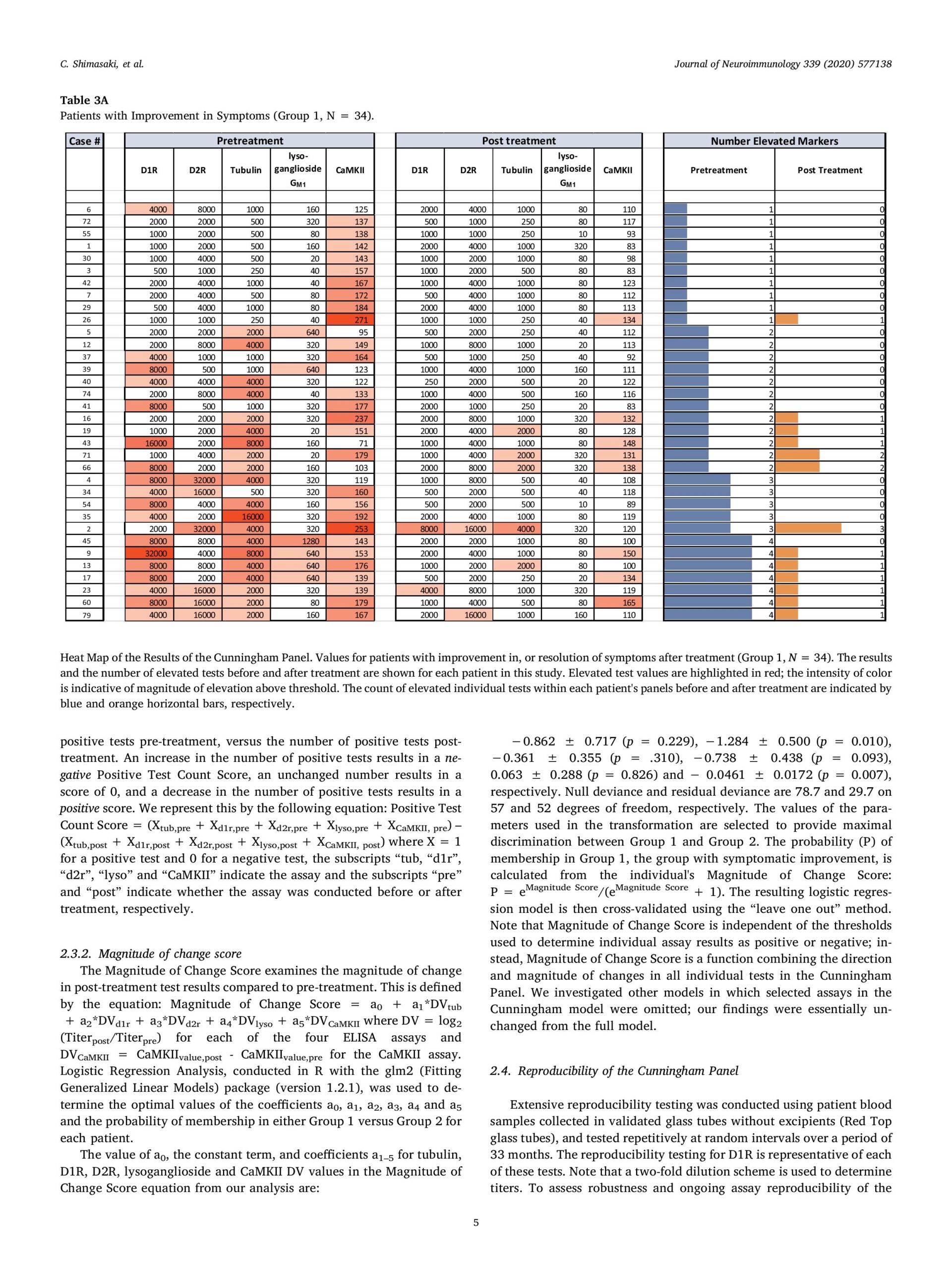
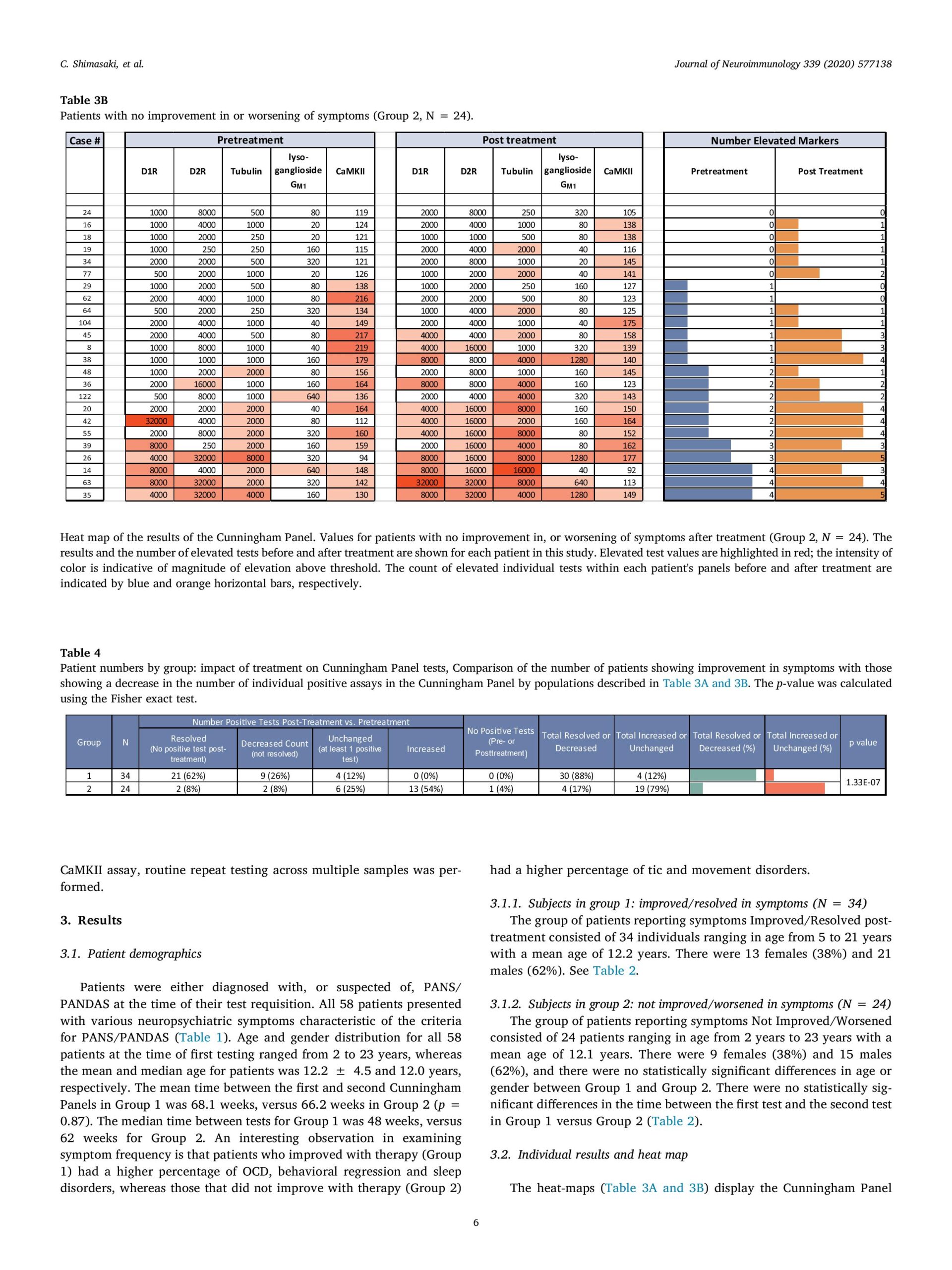
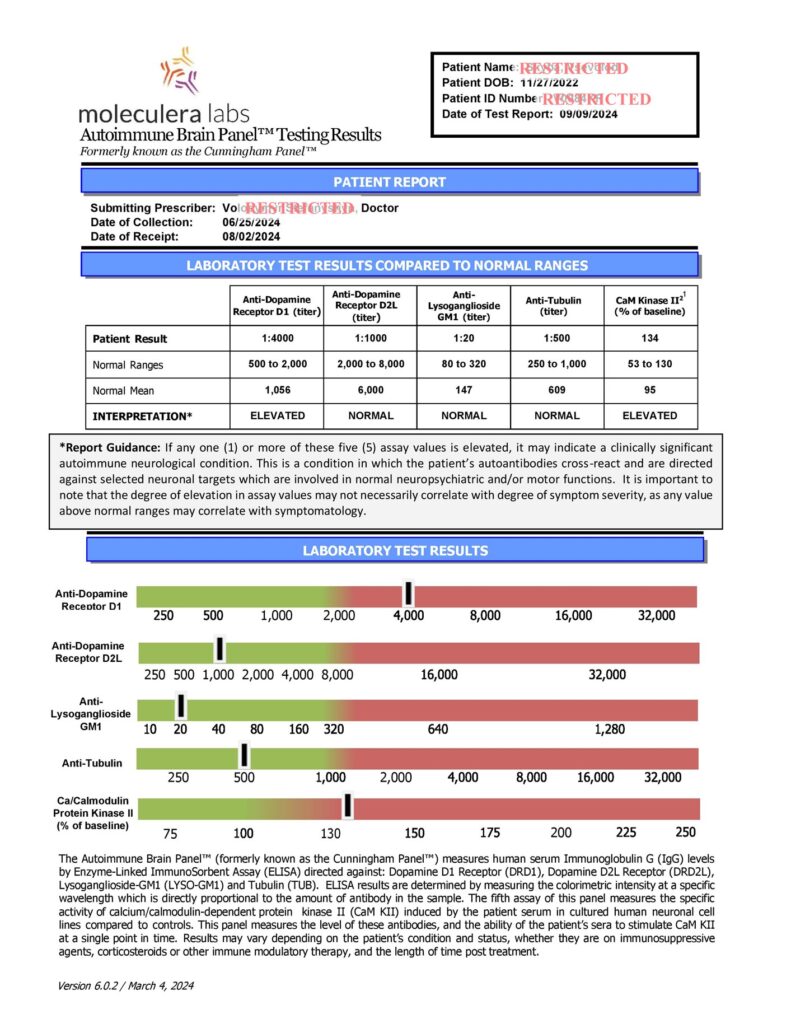
The Autoimmune Brain Panel™, previously referred to as the Cunningham Panel™, is a specialized blood test used to help diagnose certain autoimmune neurological and psychiatric disorders, particularly in children and adolescents. It’s most commonly associated with PANS (Pediatric Acute-onset Neuropsychiatric Syndrome) and PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections).
What is the Autoimmune Brain Panel™ ?
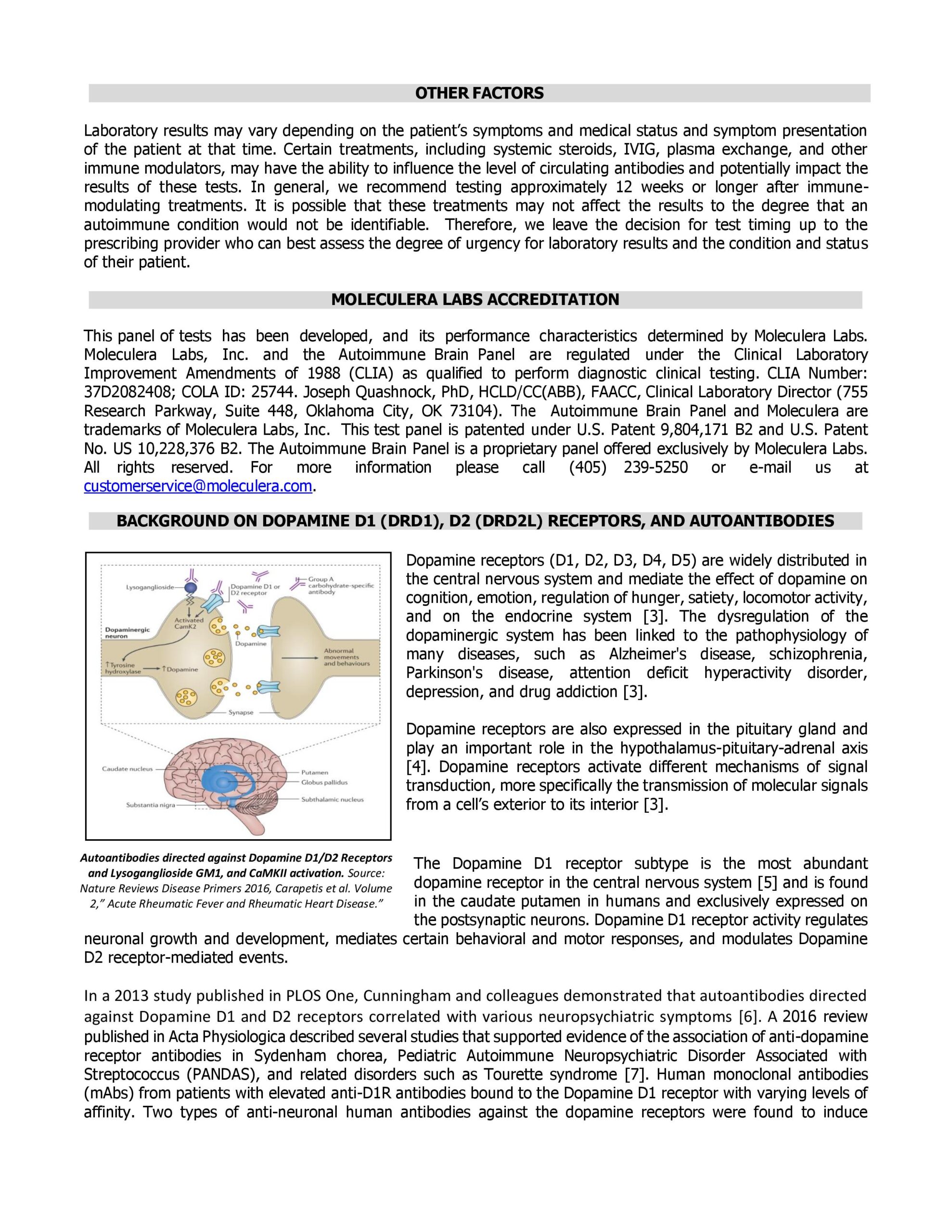
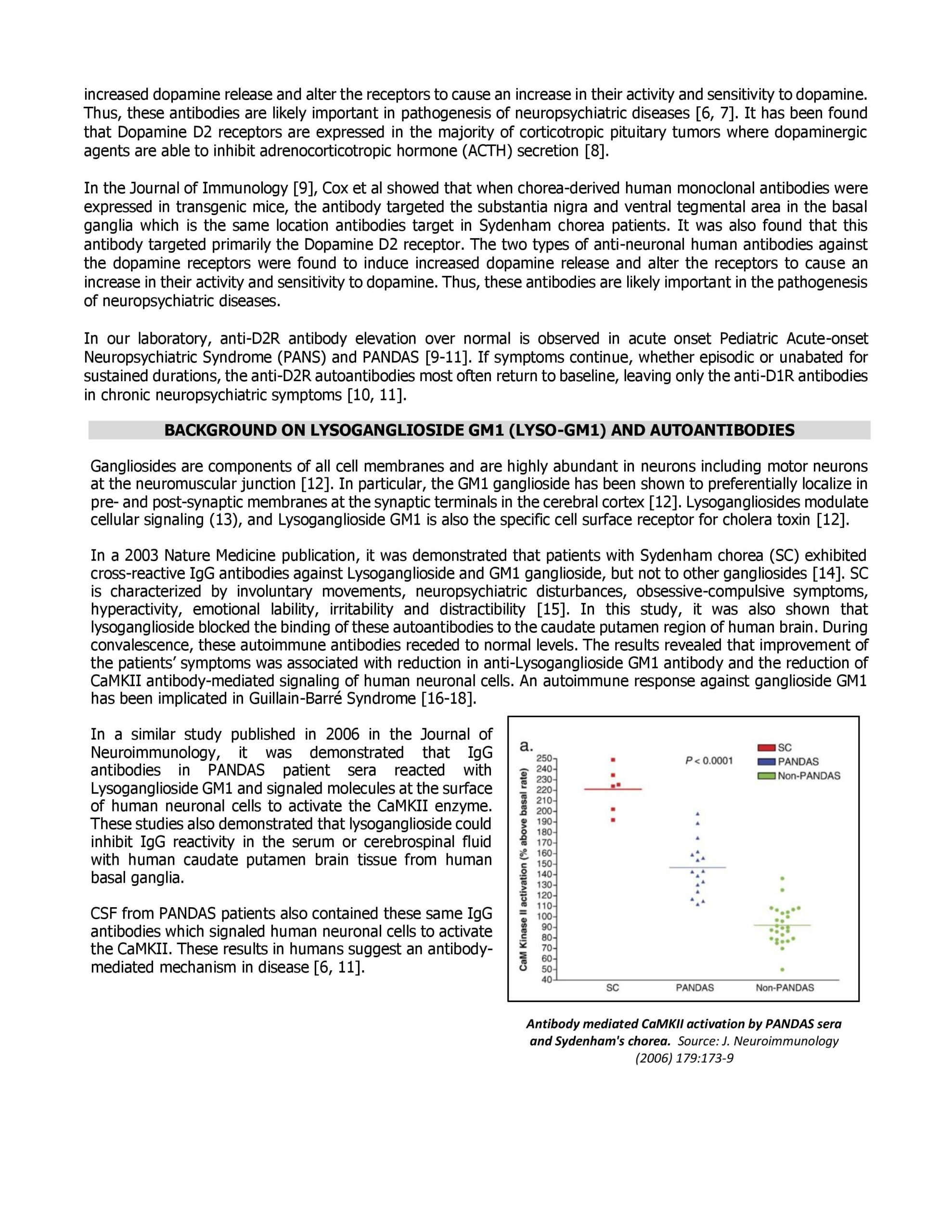
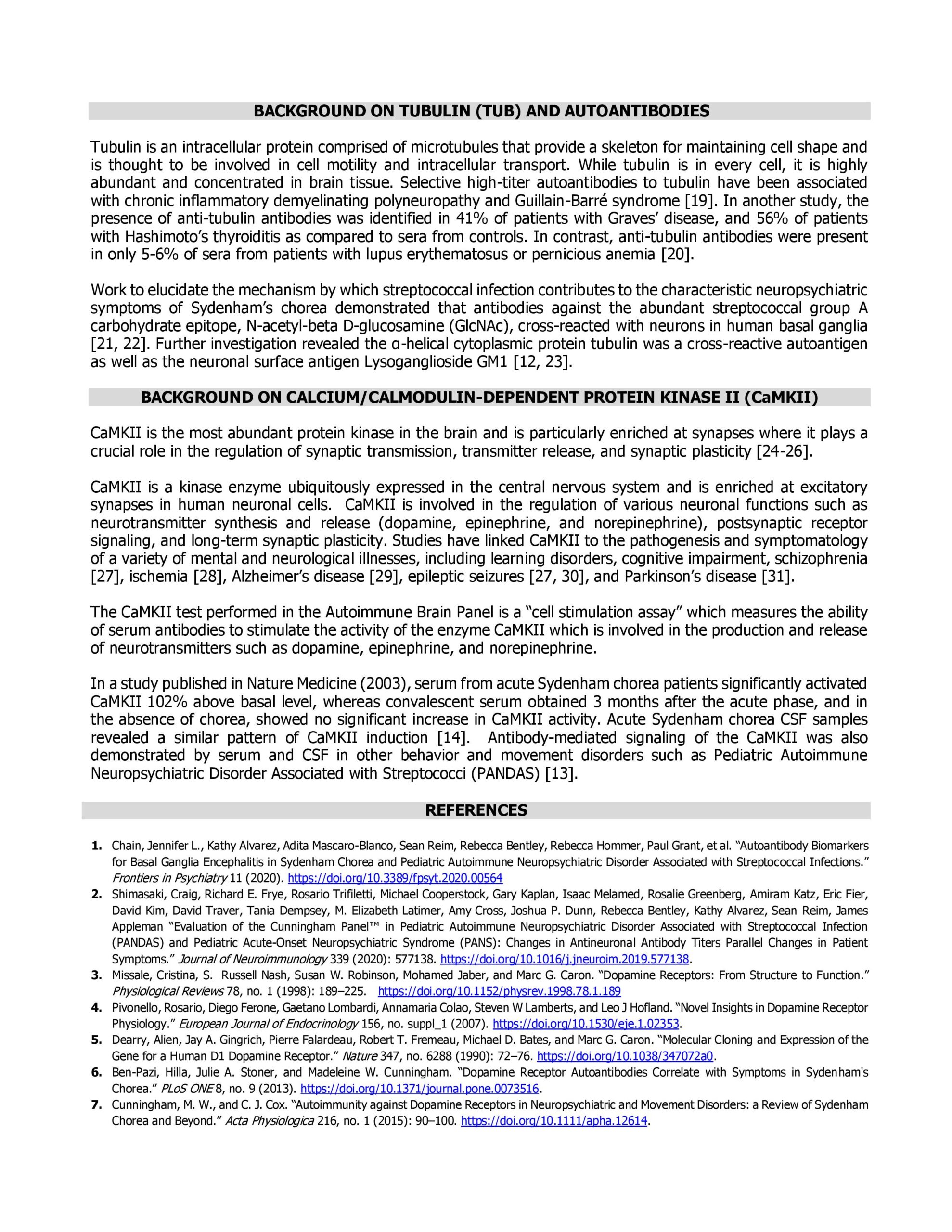
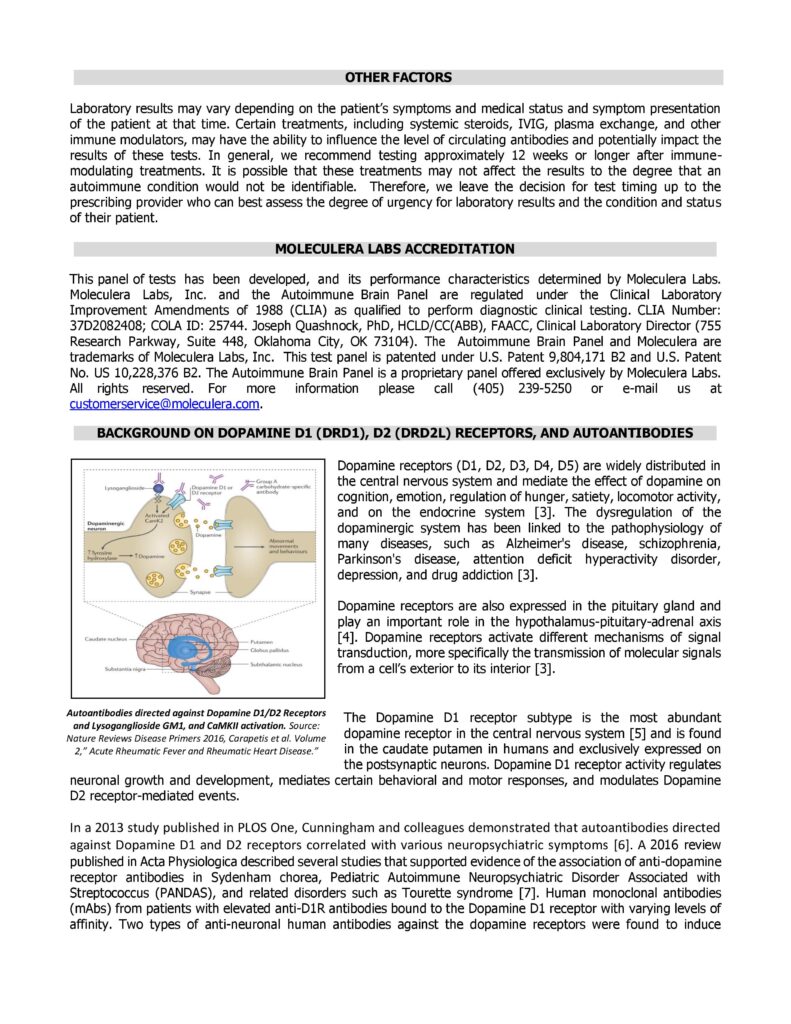
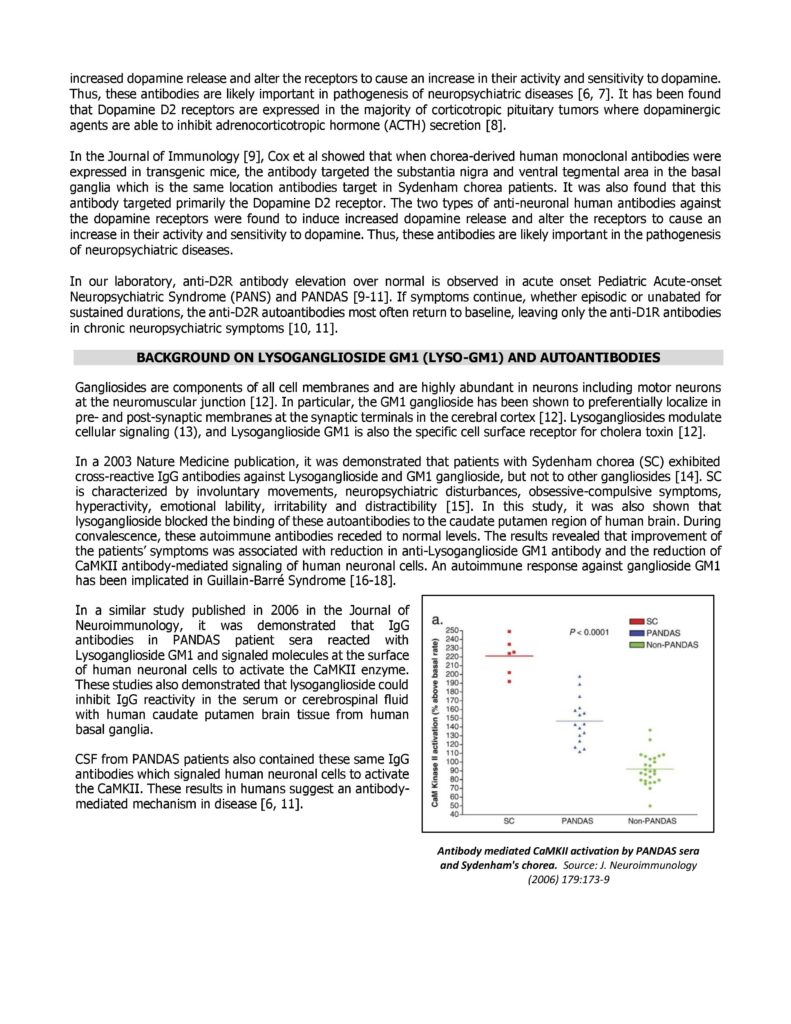
The Autoimmune Brain Panel™ measures levels of autoantibodies and the activity of certain immune-related markers that may indicate an autoimmune attack on the brain — especially in the basal ganglia, a region involved in movement and behavior.
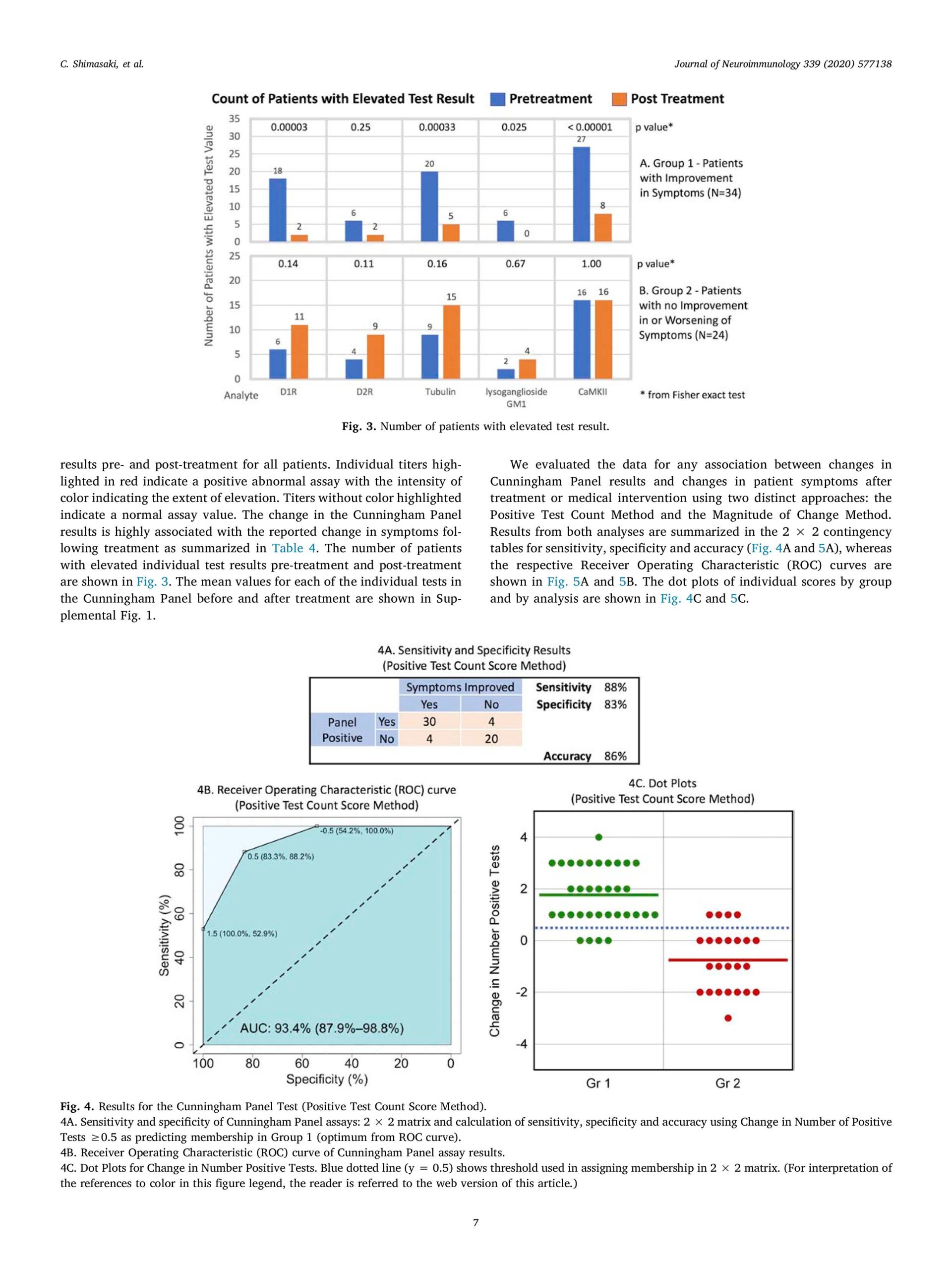
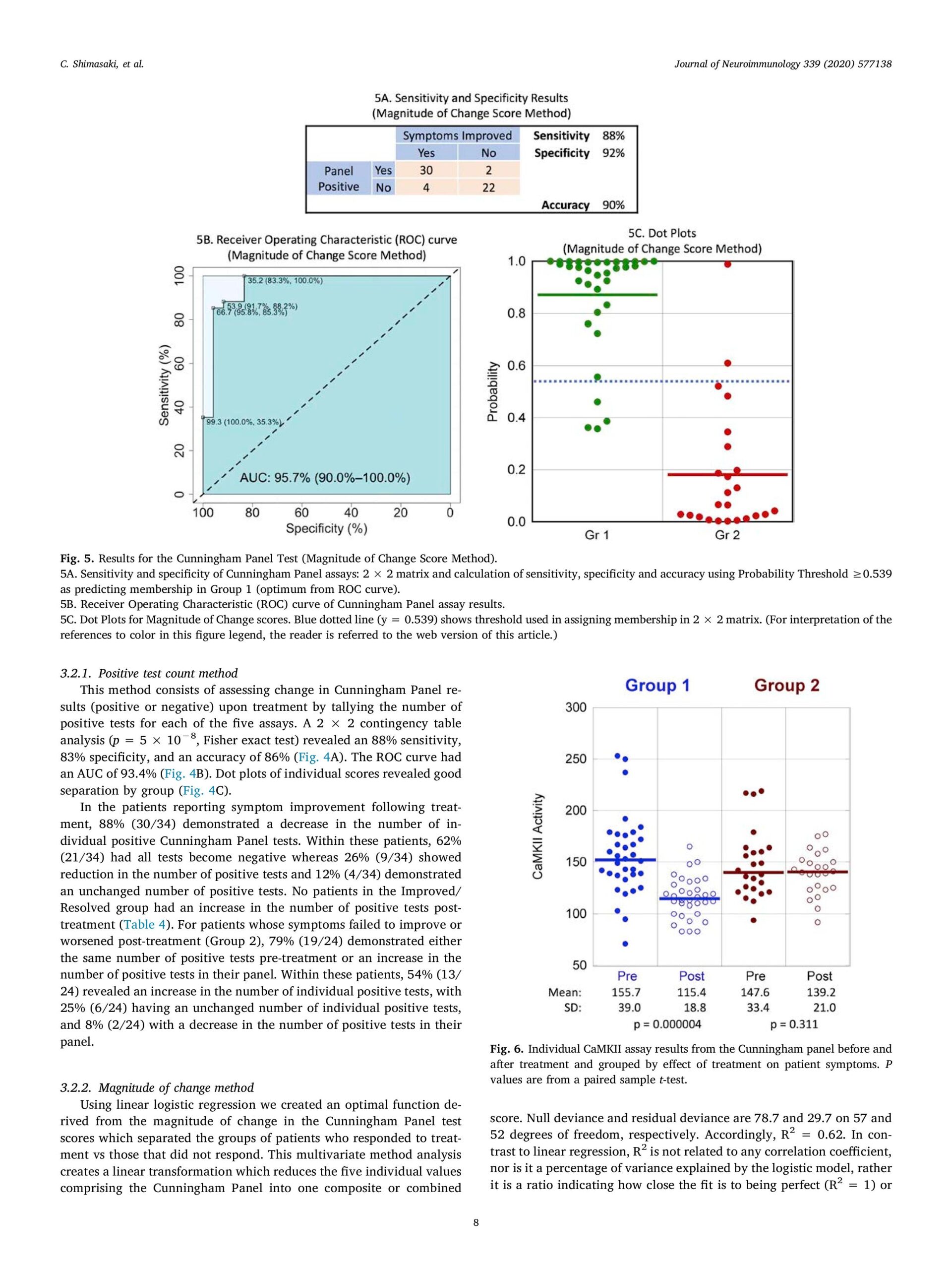
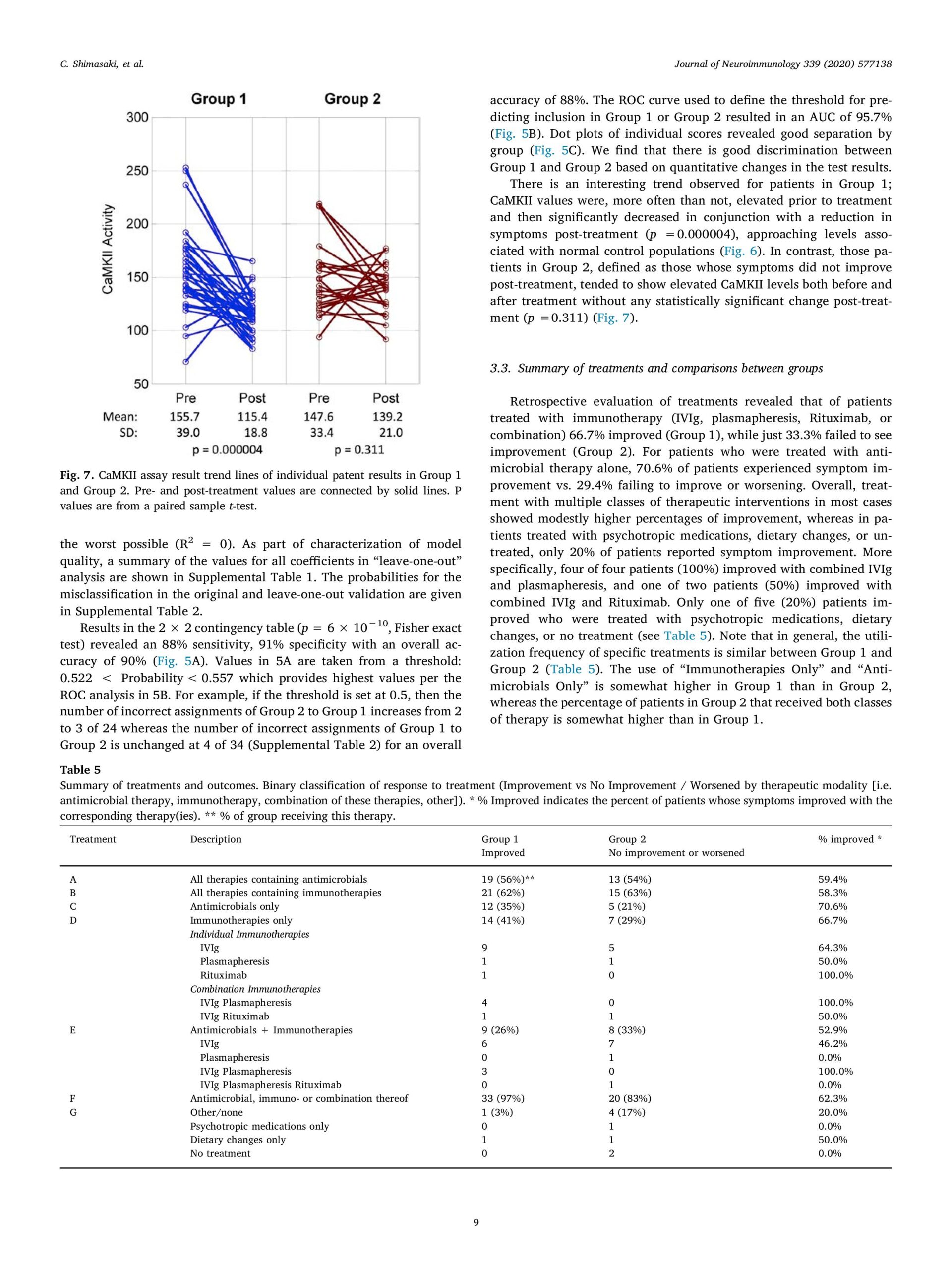
The panel typically includes five key markers:
1. Anti-Dopamine D1 Receptor Antibodies
2. Anti-Dopamine D2L Receptor Antibodies
3. Anti-Lysoganglioside GM1 Antibodies
4. Anti-Tubulin Antibodies
5. CaMKII (Calcium/Calmodulin-dependent Protein Kinase II) Activation – reflects the overall immune activation affecting neuronal function.
These markers are often elevated in children with suspected PANS/PANDAS, indicating that the immune system is mistakenly targeting parts of the brain.
Why is the Autoimmune Brain Panel™ important for children with orphan diseases?
1. Identifies Possible Autoimmune Causes
Some rare (orphan) diseases involve the immune system attacking the brain — this is known as autoimmune encephalopathy. Autoantibody testing helps detect these immune responses, which may otherwise go unnoticed.
2. Explains Sudden or Unusual Symptoms
In children with orphan diseases who develop sudden changes in behavior, movement, mood, or cognition, tests like the Cunningham Panel can help determine whether autoimmunity is involved.
3. Guides Treatment Choices
If an autoimmune process is detected, doctors may consider immunotherapy treatments (like IVIG, steroids, or plasmapheresis) — which can be effective in improving symptoms. This approach differs significantly from standard treatments for genetic or neuropsychiatric disorders.
4. Reduces Diagnostic Uncertainty
Children with orphan diseases often face long, complex diagnostic journeys. Autoantibody testing can add an important piece to the puzzle and help physicians build a more complete picture of the child’s condition.
5. Supports Personalized Care
Knowing whether an autoimmune process is involved allows for more tailored, multi-disciplinary care, involving neurology, immunology, psychiatry, and genetics.
For some children with orphan diseases — especially those with unexplained neuropsychiatric symptoms — the Autoimmune Brain Panel™ and similar autoantibody tests can reveal hidden autoimmune activity and open new treatment pathways.
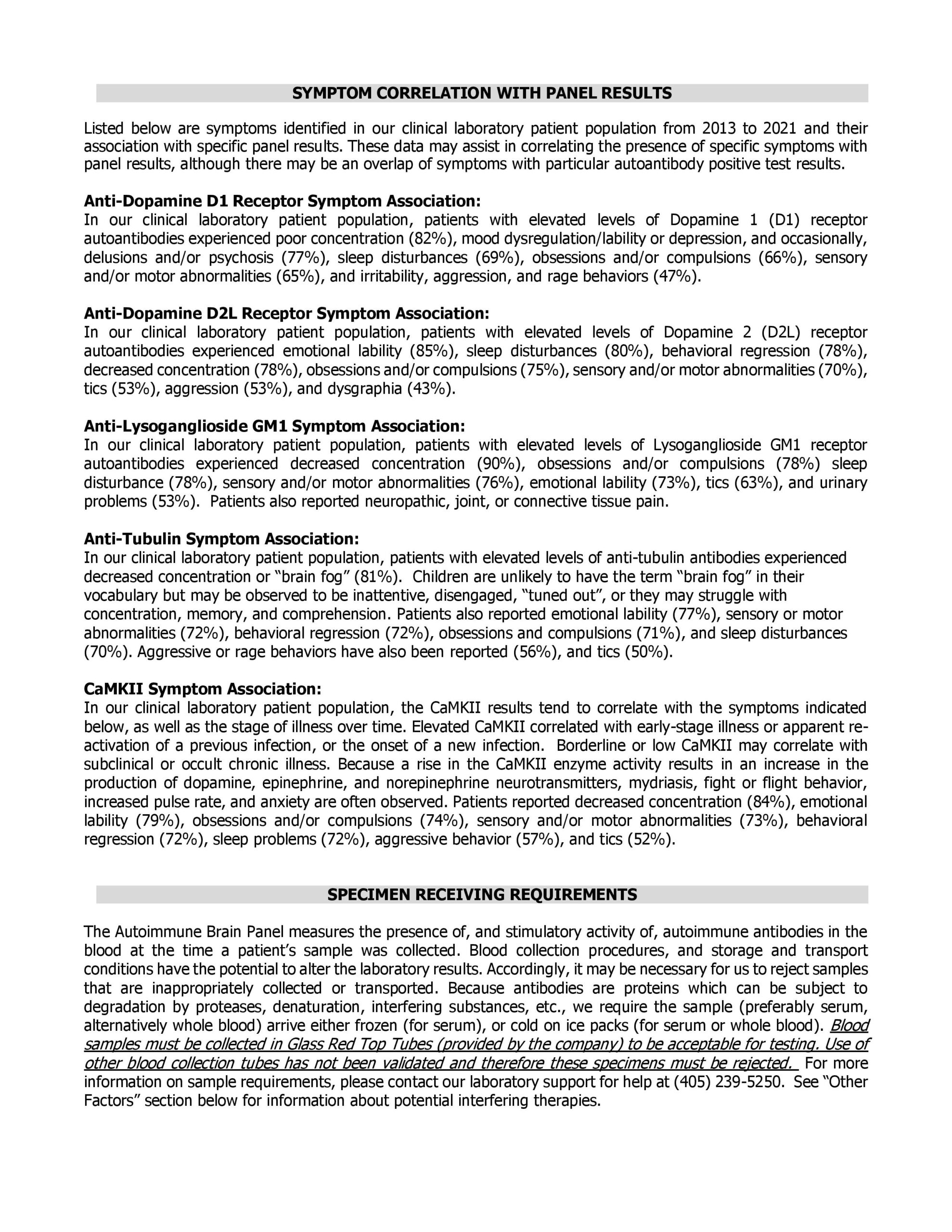
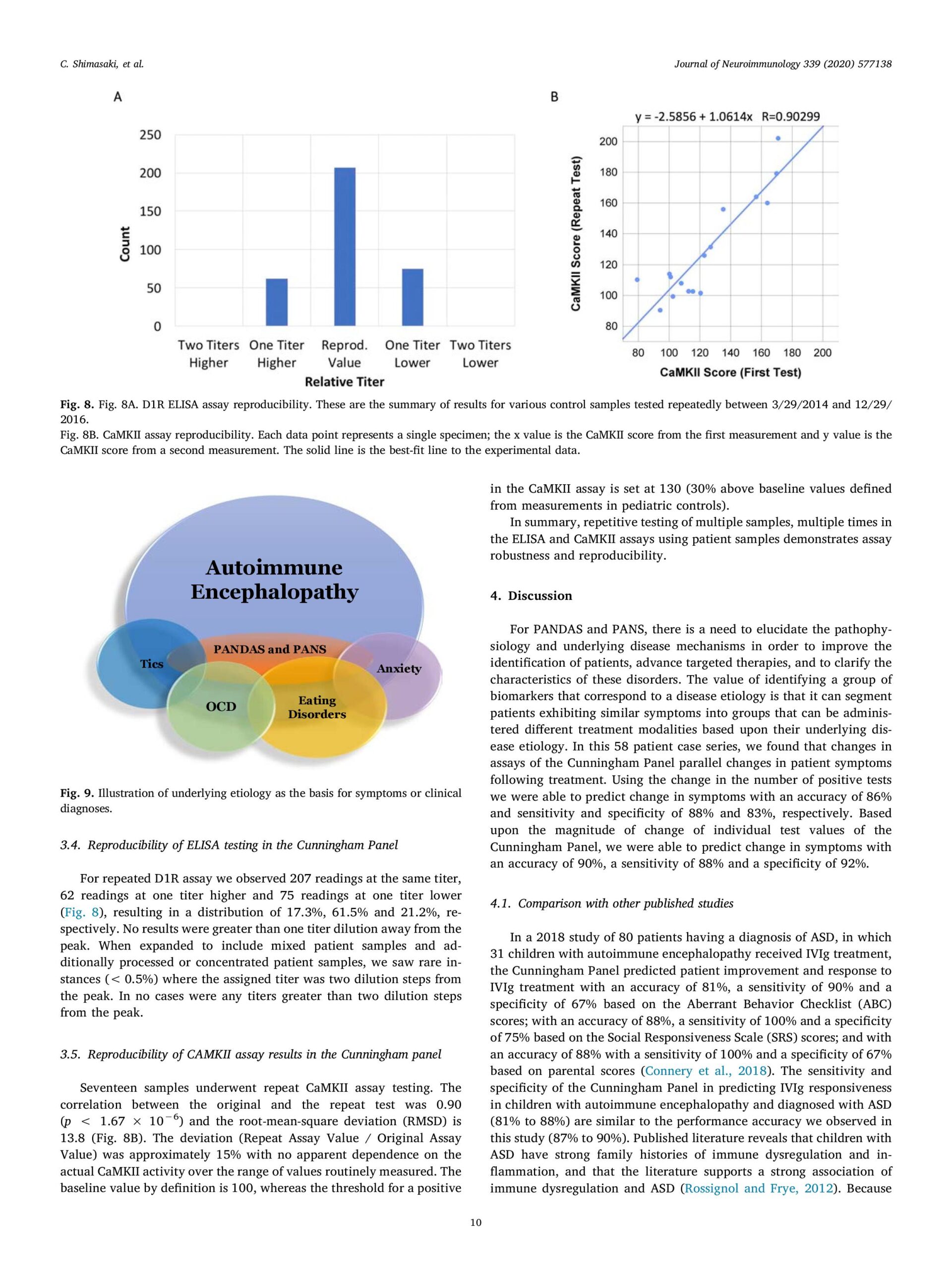
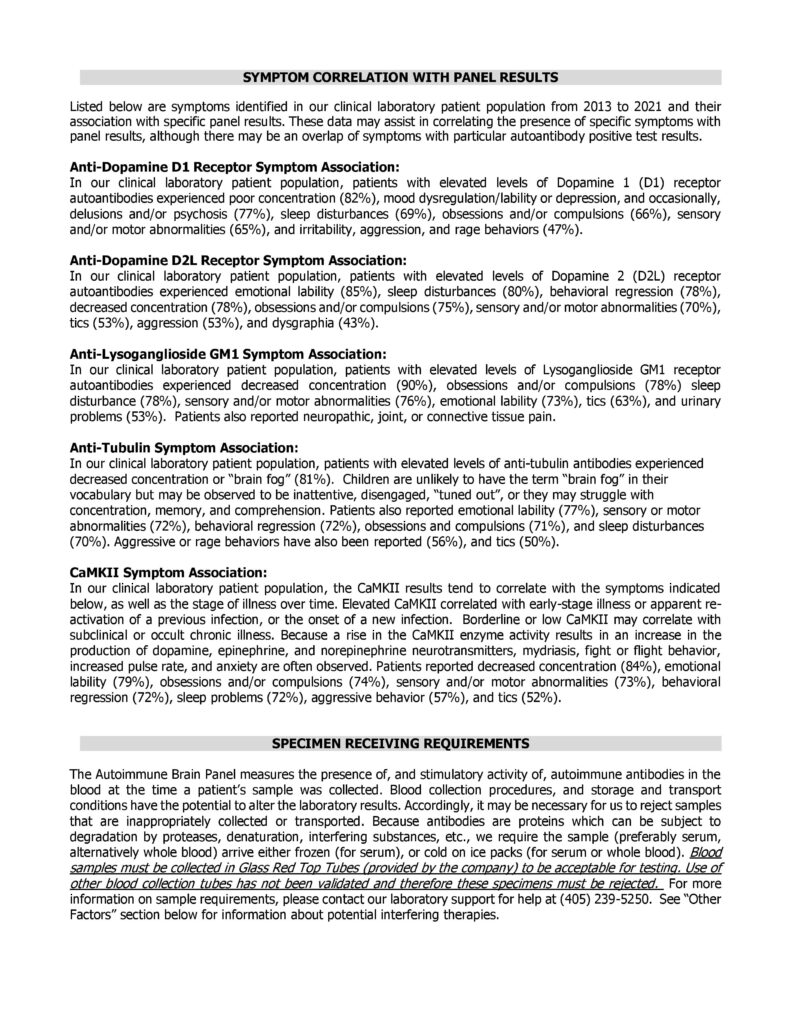
What conditions is the Autoimmune Brain Panel™ most commonly used for?
- To support the clinical diagnosis of PANS or PANDAS
- To determine if a child’s neurological or psychiatric symptoms (such as OCD, tics, anxiety, behavioral regression, or motor issues) may have an autoimmune cause
- To guide treatment decisions, including immunomodulatory therapies like IVIG, corticosteroids, or antibiotics













Autoimmune Brain Panel™ is not a stand-alone diagnostic tool — it supports, but does not replace, clinical evaluation. Although it remains controversial in some medical communities — as research is ongoing and some clinicians question its specificity — the Autoimmune Brain Panel™ is gaining increasing popularity in Ukraine, particularly among families of children with suspected autoimmune neurological conditions.
In Ukraine, this test is not performed locally. Biological samples are collected and shipped to the United States through accredited medical institutions. The test is then analyzed by Moleculera Labs, a specialized laboratory based in the US that developed and offers the Autoimmune Brain Panel™
Step-by-Step Procedure: Autoimmune Brain Panel™ from Ukraine to the US
- Medical Evaluation & Referral
A Ukrainian physician evaluates the child and determines whether the Autoimmune Brain Panel™ is clinically indicated.
- Sample Collection in Ukraine
Certified medical institutions in Ukraine collect the required blood samples using approved protocols and materials.
- International Shipping to the US
The biological samples are securely packaged and shipped to the certified US laboratory in compliance with international medical transport standards.
- Laboratory Testing & Analysis
The panel is processed at the US lab, where specialized tests are performed to measure key biomarkers related to autoimmune neuropsychiatric conditions.
- Results & Clinical Interpretation
Within several weeks, the results are returned and interpreted by qualified specialists, with recommendations provided to the referring physician in Ukraine.
Medical service cost
In Ukraine, the Autoimmune Brain Panel™ is offered at a cost of $1,100, including sample collection, logistics, and international shipping.
It is typically performed at least twice as part of a comprehensive clinical protocol. The initial test serves a diagnostic function, establishing the patient’s baseline immunological profile. A follow-up test is usually conducted after the completion of an immunomodulatory or other therapeutic intervention, in order to evaluate the patient’s response to treatment and inform further therapeutic decisions. Thus, the program includes two tests per child, with a total cost of $2,200 per case.
The total project cost of Autoimmune Brain Panel™ Program for 5 Ukrainian children is $11,000
Due to its high cost, both physicians and parents are often forced to seek assistance from charitable foundations in order to make the testing accessible for children in need.
Justification for the Cross-Border Autoimmune Brain Panel™ Program
1. The child remains safely in Ukraine
All necessary medical procedures — including sample collection and initial evaluation — are conducted in-country, eliminating the need for international travel. This is especially critical during wartime or for children with unstable health conditions.
2. Parents are spared the logistical and financial burden of overseas care
Families are not required to navigate the complex and often costly process of obtaining medical visas, arranging international transportation, or covering accommodation expenses abroad. This significantly reduces emotional and financial stress for already-vulnerable households.
3. All medical logistics are coordinated locally and professionally
Our team oversees the entire process — from medical referral and sample collection to international shipment and communication with the U.S. laboratory. We work exclusively with certified Ukrainian clinics and follow strict quality assurance protocols at every step.
4. Full transparency and child-centered care
Every aspect of the program is designed with the child’s best interests in mind. We ensure accountability, medical accuracy, and clear communication with families and healthcare providers. Our goal is to deliver not only diagnostic clarity, but also dignity, compassion, and peace of mind.

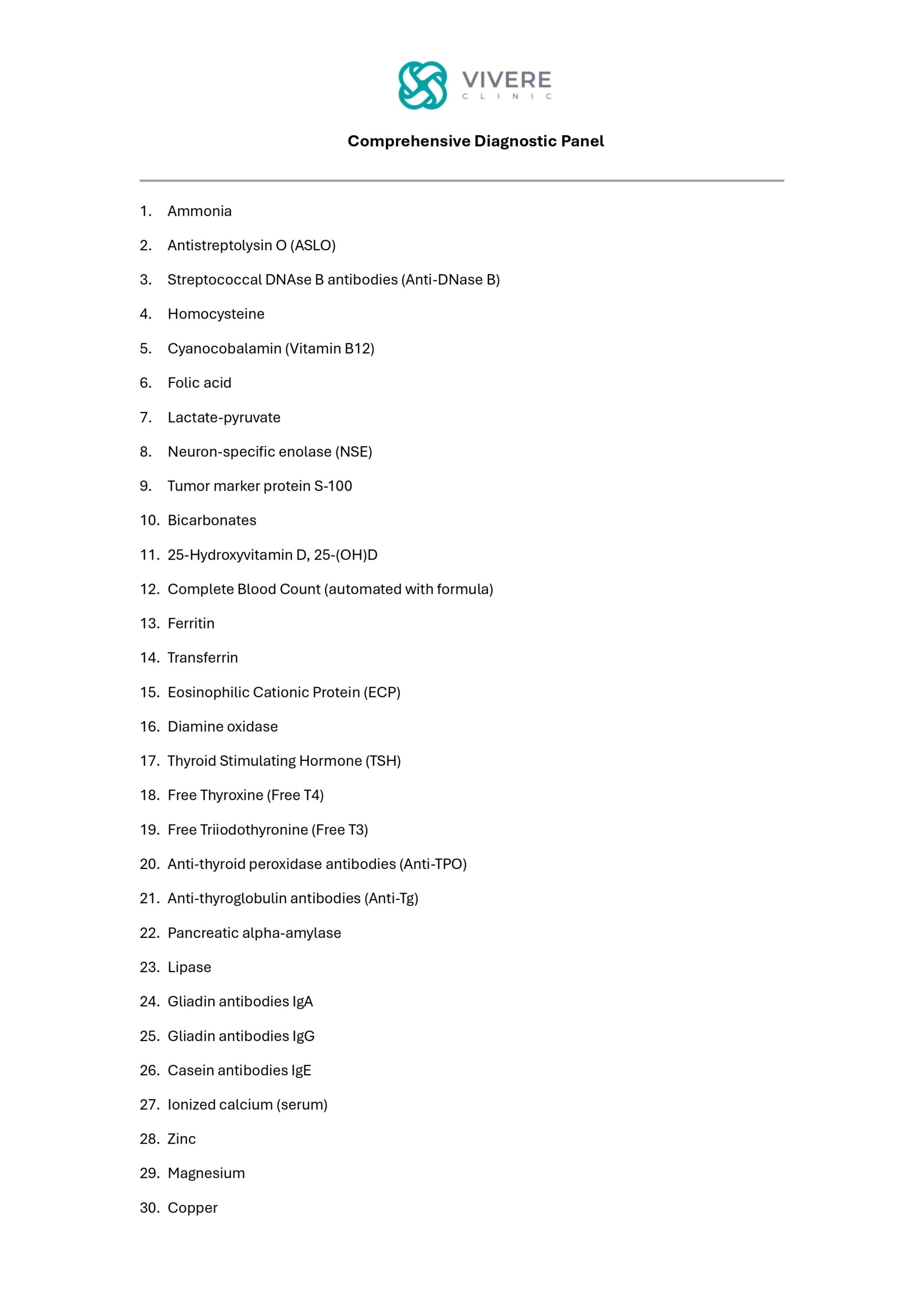
2025 – CDP (Comprehensive Diagnostic Panel)
An Essential Tool for Multidisciplinary Healthcare
Multidisciplinary (or interdisciplinary) healthcare is an approach where specialists from different medical fields work together to assess and treat the patient as a whole, rather than focusing narrowly on a single organ system or symptom. Unlike classical medicine, which is often fragmented by specialties, this model integrates diverse expertise to provide comprehensive, coordinated care tailored to the patient’s overall condition.
Multidisciplinary healthcare in diagnosing and treating rare diseases is critically important because such conditions are often complex, affect multiple systems of the body, and are difficult to identify within a single specialty. A collaborative team of experts—neurologists, geneticists, immunologists, endocrinologists, clinical psychologists, etc.—can pool their knowledge, ensuring faster and more accurate diagnosis.
Advantages:
- Holistic perspective: avoids fragmented care by considering the patient’s entire condition.
- Higher diagnostic accuracy: rare diseases often present overlapping or atypical symptoms that require cross-specialty expertise.
- Timely intervention: reduces diagnostic delays (“diagnostic odyssey”), improving chances of effective treatment and quality of life.
- Personalized care plans: coordinated input leads to tailored therapies and support, addressing both medical and psychosocial needs.


Justification for the Comprehensive Diagnostic Panel (CDP)
The Comprehensive Diagnostic Panel (CDP) is a universal and indispensable diagnostic tool, consisting of 52 essential laboratory tests. Unlike traditional diagnostic approaches—where individual specialists order separate tests in sequence—the CDP provides a holistic dataset from the outset. This integrated approach allows all members of a multidisciplinary medical team (e.g., pediatricians, neurologists, geneticists, endocrinologists, psychiatrists, and others) to simultaneously access the same comprehensive clinical information.
Advantages of the CDP:
- Efficiency & Time-Saving – Reduces diagnostic delays by eliminating fragmented or repeated testing across specialties.
- Cost-Effectiveness – Prevents duplication of tests and unnecessary hospital visits, optimizing healthcare resources.
- Accuracy & Early Detection – Enhances the precision of diagnosis, especially for rare and complex disorders, by capturing multi-system data at once.
- Holistic Care – Facilitates truly integrated patient management, ensuring that treatment strategies are based on a complete understanding of the child’s condition.
- Family-Centered Benefits – Minimizes stress and financial burden on families, who otherwise face long diagnostic journeys.
- Minimized & Single-Site Blood Sampling – Single-site blood sampling for the CDP minimizes physical discomfort and stress for children by reducing the number of required visits and blood vials. The program ensures complete data collection in a single session.
Instead of requiring multiple visits to different laboratories and 20–25 separate vials of blood, the CDP requires only one visit and 15 vials. This significantly reduces physical discomfort, psychological stress, and medical risks for children, while ensuring complete data collection in a single session.
This advantage is particularly critical for children with special needs, for whom every hospital visit and blood draw can represent a tremendous challenge, severe stress, and even a form of trauma—both for the child and for their parents.
By consolidating the process into a single, minimized procedure, the CDP greatly alleviates the emotional and logistical burden on families while ensuring the highest quality of care.
The Current Adverse Situation in Ukraine
Unfortunately, there is not a single state medical institution—including the National Children’s Hospital “Okhmatdyt”—capable of performing such a comprehensive panel. In fact, many of the included tests are not conducted in Ukraine at all and must be sent abroad for processing. Some of the rarest and most exclusive analyses are available only through highly specialized laboratories overseas. As a result, families of children with special needs are left with no choice but to turn to private clinics, the availability of which remains extremely limited in Ukraine.
While the CDP’s cost of $1,100 per person is justified, it is prohibitively high for most Ukrainian families. This is especially true for families raising children with special needs, who already face immense financial burdens from medical care, rehabilitation, and educational expenses.
To ensure equitable access to the CDP for children with rare and unspecified diseases, we are offering a program specifically tailored for this vulnerable group.
This initiative will cover the full cost of the program for 10 children, totaling $11,000
Ultimately, our goal is to leverage the Comprehensive Diagnostic Panel (CDP)—a truly universal and indispensable diagnostic tool—to advance the principles of multidisciplinary healthcare for Ukraine’s most vulnerable children.
The CDP is more than just a set of tests; it is the foundation for an integrated, collaborative approach to care. By providing this vital tool, we can ensure that children with rare and unspecified diseases receive the accurate, holistic diagnosis they desperately need. This is a critical first step in their journey towards effective treatment and a better quality of life.

Educational and Corrective Programs
2025 – Special Needs Provider (SNP) – in-home caregivers
Empowering Children Through Specialized Support
Investing Today to Prevent Lifelong Exclusion
Due to the ongoing war, a significant number of children with special educational needs have been compelled to transition to distance or home-based learning. In this context, the burden of ensuring access to quality education has shifted largely to parents, who are often required to engage and finance the services of Special Needs Providers (SNP).
These professionals are highly qualified and in limited supply within Ukraine, making their services both difficult to access and financially burdensome for many families. As a result, an increasing number of parents turn to our charitable foundation seeking support in locating and covering the costs of such essential specialists for their children’s continued learning and development.
Providing access to correctional educators is a key component of our Inclusive Development Program for children with special educational needs, which our foundation actively promotes and implements. This program aims to ensure that every child, regardless of their circumstances, receives the individualized educational support they need to thrive.

Unfortunately, and especially during wartime in Ukraine, the system of social workers — who would otherwise help families of children with special needs cope with the enormous daily burden — is virtually non-existent. While specialized educational institutions do exist, they are severely underfunded and face an acute shortage of qualified personnel. Even when a child attends such a center, it typically operates only until midday, leaving parents with no choice but to leave work early or hire private specialists at their own expense.
For low-income families and single-parent households, this becomes a crisis that affects not only the child, but also their siblings and already exhausted caregivers. As one mother put it: “I have to give my salary to an educator so I can keep my job.”
The issue is so widespread, and the demand for qualified specialists is so diverse and urgent, that our program is built around average benchmarks and indicative cost estimates. At the same time, for each individual child, we help identify, train, and fund the services of a dedicated professional who is best suited to meet that child’s unique medical and educational needs.

For the purposes of this program, we use the term Special Needs Provider (SNP) as a general designation for all professionals involved in supporting children with developmental, cognitive, and physical challenges. We distinguish three main categories of specialists within this framework:
- Special Education Teacher – professionals trained to support school-age children with learning, behavioral, developmental difficulties or physical disabilities. This category includes remedial teachers, who help close learning gaps in core academic areas; inclusive education specialists, who adapt curriculum and classroom practices to meet diverse needs; tutors, who provide individualized instruction to reinforce progress and ensure continuity of learning across settings; home-based educators, who work individually with a child in the home setting to provide personalized academic instruction and developmental support etc.
Their role includes:
- Assessing students’ individual needs
- Developing Individualized Education Plans (IEPs)
- Providing tailored educational support
- Using special teaching methods and tools
- Collaborating with parents, therapists, and other educators
- Supporting social, emotional, and communication development
- Early Childhood Educator (with specialization in developmental delays) – specialists working with young children to support early cognitive, speech, and social development. This category includes correctional psychologists who address developmental and behavioral challenges; speech therapists (logopedists) focusing on speech and language improvement; and ASD specialists providing targeted support for children on the autism spectrum.
This issue is particularly urgent in Ukraine, where many parents—often due to lack of information, stigma, or limited access to services—do not seek timely support for their child’s developmental delays. Hoping that the child will simply “grow out of it,” they miss a critical window for early intervention. As a result, the challenges become significantly more severe by the time the child reaches school age, often leading to long-term disability and exclusion from mainstream education.
- Caregiver/Nanny/Nurse Aide – individuals providing essential daily support, supervision, basic care, and physical assistance, including hygiene or basic medical support when needed (e.g., by a nurse or aide). Beyond practical tasks, they offer crucial emotional support and stability for the child, helping reduce stress and behavioral challenges. These professionals often accompany the child to therapies, school, or medical appointments, ensuring continuity of care. In many cases, they serve as a vital bridge between home and educational or therapeutic environments, significantly easing the burden on parents and other family members.

Cost of Special Needs Providers’ Services
The average cost of hiring a qualified specialist to support a child with special needs is approximately $750 per month, or $9,000 per year, covering the salaries of dedicated Special Needs Providers (SNPs) who work directly with each child and their family.
The Program designed to support 10 families would therefore require an annual budget of $90,000
Despite the high cost, the presence of qualified Special Needs Providers is absolutely critical.
These professionals are often the only bridge between a child with developmental challenges and any meaningful chance at education, communication, social integration, and a dignified life. Without their support, children are at significant risk of long-term institutionalization, social exclusion, and irreversible developmental setbacks.
Investing in these specialists is not just a matter of care — it is a matter of human rights, prevention, and long-term social impact. Every dollar spent today prevents far greater emotional, social, and financial costs tomorrow.

2025-30 – Inclusive Preschool
Program Designed for the Reconstruction, Equipping, Staffing, and Personnel Training of a Full-Scale Inclusive Preschool for Children with Developmental Disabilities, Focused on Early Intervention, within a State Educational Complex (School and Kindergarten) in the Kyiv Region
⚙️ This page is temporarily unavailable.
We’re updating the content to serve you better.
Please check back in a few days. Thank you for your patience!
2025-28 – Capacity Building for Special Needs Providers (SNP) Working with Children with Developmental Disabilities
Educational and Professional Development Program designed for tutors, school teachers, preschool educators, staff of specialized medical institutions, social workers, and in-home caregivers
⚙️ This page is temporarily unavailable.
We’re updating the content to serve you better.
Please check back in a few days. Thank you for your patience!
Research Grant Programs
2025-28 – Children with ASD: Genetic, Metabolic, Immunological, and Epigenetic Factors
Research Grant Program for a Three-Year Scientific Study within a PhD Thesis: ‘A Personalized Medicine Framework for the Diagnosis and Treatment of Children with Autism Spectrum Disorders: Integrating Genetic, Metabolic, Immunological, and Epigenetic Determinants’
⚙️ This page is temporarily unavailable.
We’re updating the content to serve you better.
Please check back in a few days. Thank you for your patience!
2025-30 – Genetics/Orphan Diseases/mTORopathy
The Program, under the auspices of the Ministry of Health of Ukraine, is designed to enhance the diagnosis and treatment of Ukrainian children with mTORopathy by uniting the expertise of leading international researchers and clinicians with the resources of the Medical and Genetic Center of the “Okhmatdyt” National Children’s Specialized Hospital.
⚙️ This page is temporarily unavailable.
We’re updating the content to serve you better.
Please check back in a few days. Thank you for your patience!